Information to help you get ready for your immunotherapy treatment
![]() Download a PDF of this guide rfsdf or (opens in a new window) or read it online below.
Download a PDF of this guide rfsdf or (opens in a new window) or read it online below.
This page will give you information about:
- What immunotherapy is
- Symptoms and side effects of immunotherapy
- What to expect on the day of treatment
- Your lifestyle during treatment
- Other services available
What is immunotherapy?
Your immune system fights infections and diseases. Immunotherapy is a type of cancer treatment (drug) that uses your body’s own immune system to fight cancer cells. Immunotherapy can fight your cancer even after your treatment ends. Sometimes this can lead to long-term control of your cancer.
What is the difference between immunotherapy and chemotherapy?
Immunotherapy makes your immune system stronger at finding and attacking cancer cells. Chemotherapy attacks cancer cells by stopping their growth and spread. Chemotherapy and immunotherapy have different side effects because they work in different ways.
How do I know which treatment is right for me?
Immunotherapy can be given for certain types of cancer and stages. If you are on immunotherapy, you may get one of two immunotherapy drugs.
How is immunotherapy given?
You will get immunotherapy through your veins using an IV (needle into the skin). As the fluid enters your veins, it may feel cool. This may cause some mild discomfort.
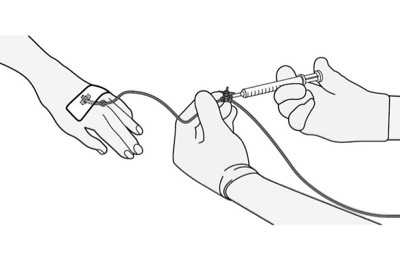 Image 1: IV
Image 1: IV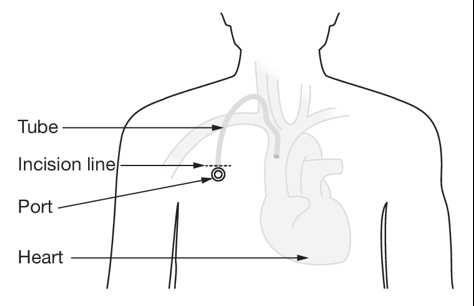 Image 2: Port
Image 2: Port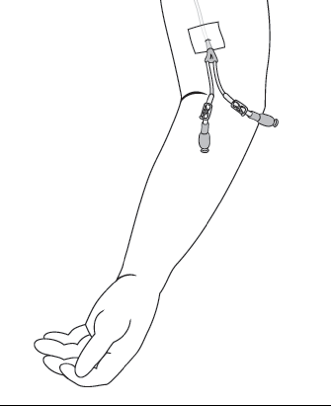 Image 3: PICC line
Image 3: PICC lineSymptoms and side effects of immunotherapy
| Common symptoms | Less common symptoms |
|---|---|
|
|
If your side effects are more than mild, your immunotherapy may be stopped for a period of time, and you may need steroids or other treatments (to suppress your immune system).
Note: Tell your doctor and nurse if you have any on-going medical issues, like autoimmune diseases (such as colitis, lupus, etc.) as these can get worse on immunotherapy.
What do I do if I have a fever?
A fever is a temperature reading in the ear or mouth of:
- 38.3ºC (100.9ºF) ONCE or
- 2 readings of at least 38ºC (100.4ºF) for one hour
Take your temperature if you feel unwell. It is best to use a digital thermometer in your mouth or ear. Avoid hot or cold foods before you take your temperature.
Note: If you have a fever, call your nursing team line or after-hours line. If you cannot reach anyone within two hours, go to your local emergency room.
What do I do if I have flu-like symptoms?
You may feel flu-like symptoms from the immunotherapy injection, such as:
- Feeling warm, with or without a fever
- Aches and pains
- Chills (feeling like you are cold and cannot get warm)
Note: If your symptoms that last more than 48 hours, call your health care team to report your symptoms.
What should I do if I have diarrhea?
Diarrhea is loose, watery bowel movements or more bowel movements that what is normal for you.
Call your health care team to report your symptoms – do not wait!
To help:
- Drink lots of fluids.
- If your bottom is sore, try a warm bath (sitz bath).
What if I am having trouble breathing?
Breathing problems means that this is swelling and irritation of the lungs (pneumonitis).
Check to see if you have:
- Trouble breathing/catching your breath
- Have new or worsening cough
- Chest pain
Note: If you have these symptoms and a fever, call your nursing line or after-hours line. If you cannot reach anyone within two hours, go to your local emergency room.
Will I have changes to my skin?
Changes to your skin are common during immunotherapy. Vitiligo is changes to the colour or texture of your skin or hair. Some immunotherapy medications can cause a skin rash or dry, itchy, uncomfortable skin.
What do I do if I have skin changes?
You can use medications suggested by your health care team to manage your skin. A topical treatment (medicine on your skin like cream or lotion) is usually tried first. If this continues to be a problem, speak to your health care team.
Other things you can do that may help:
- Wear sunscreen and a hat.
- Try to stay away from the heat and cold.
Will I have changes to my hair?
Most patients do not have hair loss when on immunotherapy. There may be changes to the colour or texture of your hair.
Ask your health care team if it is safe to colour your hair or use dye products.
What are hormonal (endocrine) side effects?
Immunotherapy can change levels of some of your hormones. Your doctor will order blood tests to check your hormone levels and liver function while you are on immunotherapy. Hormonal changes can be related to your thyroid, adrenal or pancreas.
How do I manage hormonal changes?
| Common hormonal changes to your thyroid | Hormonal changes to your adrenal and pancreas function |
|---|---|
|
|
Note: Call your health care team to report your symptoms. If you cannot reach anyone within 2 hours, go to your local emergency room.
What do liver changes feel like?
Inflammation or irritation of the liver is usually noticed on blood work by your doctor. It often means that immunotherapy has to be stopped (for a short period of time or completely depending on how severe it is). Steroids are often given to help treat swelling of the liver.
Signs of more severe liver irritation include: bloated belly, dark urine, yellow eyes or skin, fatigue, nausea, vomiting.
Note: If you have these symptoms, call your nursing team line or after-hours line. If you cannot reach anyone within TWO HOURS and the symptoms are sudden, go to your local emergency room.
Will I feel tired?
Cancer and cancer treatment can cause fatigue. Immunotherapy can also cause fatigue by causing inflammation in organs (swelling). You should always report fatigue to your health care team
The feeling of fatigue is more than just feeling tired, and does not always go away after a good night’s sleep. Exercise, such as walking each day, can help.
To learn more about fatigue:
- Download the fatigue symptom management guide.
- Watch the video on fatigue on: sunnybrook.ca/cancer-fatigue.
What about less common side effects?
Less common side effects of immunotherapy include:
- Vision changes (eyes)
- Weakness in limbs or face, confusion, headache (brain/spinal cord)
- Weakness in limbs or face, nerve pain (nerves)
- Chest pain, shortness of breath (heart)
Note: Talk to your health care team about any new symptoms, especially if they are unusual for you or sudden. They can help decide if it is from immunotherapy, your cancer, or something else.
How do I contact my health care team?
If you have these symptoms and side effects, or if you are unsure if your symptoms are from immunotherapy or from your cancer, call your health care team.
Call the nursing line:
- Monday to Friday, between 8:30 a.m. – 4:30 p.m. – at 416-480-5000.
- On weekdays between 4:30 p.m. – 8:30a.m. and on weekends and holidays – call 1-877-681-3057.
- If the nurse can’t take the call right away, you will get a call back within 15-20 minutes.
What to expect on the day of treatment
Where is my treatment?
Many patients will get their immunotherapy at the cancer centre.
Depending on your insurance coverage, you may get the treatment at an outside centre (e.g. Bayshore clinic). If this is the case, you would still see your doctor before each treatment and get blood work at the Odette Cancer Centre.
Can I drive myself?
- First time – Try to get a drive with someone that lives in the same household
- Each person reacts differently to a new drug.
- Always have a backup plan/driver.
- After your first treatment –it is your choice.
If you need help getting to your appointment, please refer to “Transportation Options”.
Do I come alone? Can I bring my kids/family/friends?
Due to COVID-19, there will be no visitors permitted at Sunnybrook, until further notice. This includes family members or companions accompanying patients to appointments or procedures.
Your friends and family can still be a part of your appointment. You may ask your health care team to call them during your appointment.
Please plan to be here for the whole day
| Check-in & registration | 5 minutes – 30 minutes |
|---|---|
| Bloodwork | Up to 30 minutes |
| Waiting area | One hour – two hours |
| Pharmacy | One hour |
The treatment process
Treatment Process I
- Immunotherapy is ordered
- Nursing assessment
- Pharmacist review
- Immunotherapy preparation
- Final check of immunotherapy
- Delivery to treatment area
Treatment Process II
- Nursing reviews immunotherapy
- Collection of medication list and interaction check
- Pharmacy reviews take home medication
- Final nursing check and discharge
How long will my blood test take?
You may have different blood tests for the type of immunotherapy you are on. The type of blood test you have can mean different wait times.
How often do I need to have my blood checked?
You will need to have it checked at the start of each immunotherapy treatment. You may not need to have blood tests for some types of immunotherapy. Your immunotherapy nurse can let you know if you need to get your blood checked.
Will I have to pay for medication?
Immunotherapy is covered by OHIP and does not have any take home medication.
You may need to pay for some supportive medication to help with side effects. There may be a cost to this.
Can I take my other pills?
You should continue to take your regular drugs as prescribed. Baby aspirin (or 325 mg daily) is allowed.
Remember:
- Bring any drugs that you take (example, pain medication, insulin) to your appointment.
- If you take any other pills like vitamins or supplements (including natural and herbal products) you should talk to your doctor, nurse or pharmacist about these before you start immunotherapy.
Do you need help on your first day?
A Companion staff will be able to help you:
- Check-in
- Get to your next destination/appointment
- Answer any questions.
You can meet them at the east entrance when you enter the Odette Cancer Centre.
Your lifestyle during treatment
Eat a well-balanced diet and drink plenty of fluids
- You can also refer to Canada’s Food guide.
- You do not need to stop eating any types of food.
Avoid alcohol
- Talk to your health care team about how to manage your alcohol use.
Quit smoking
- Quitting smoking helps your cancer treatment and how you do with treatment. Talk to your health care team if you’re interested in or are using cannabis products.
Exercise is important
- Moderation is key. Listen to your body. Talk to your doctor if you have questions about exercise and fitness.
Work
- Talk to your doctor and employer if you can continue to work.
What about my sexual health?
Cancer and immunotherapy can affect how you feel about your body and about sex. Many cancer treatments are not safe for people who are pregnant. If you are planning a pregnancy please talk to your doctor.
- Use condoms to protect your partner’s skin when having sex (vaginal, anal and/or oral).
- Talk to your health care team if you have questions.
Other services available
Many services are available as part of your care.
Patient & Family Support
- Clinical nutrition
- Occupational health
- Physiotherapy
- Social work
- Drug reimbursement
- Psychology & psychiatry
- Art therapy
- Speech language therapy
You can contact them by visiting their office located on the Ground floor, T-wing or call them at 416-480-4623.
Patient & Family Education
They have information about:
- Cancer, symptoms and side effects
- Cancer treatments
- Sexual health and cancer
- Free community programs and support groups
You can contact them by emailing patienteducation@sunnybrook.ca or calling 416-480-4534.






