Abstracts
Notable advances and achievements
International Impact

Photo: Courtesy of Fatima Gabolaeva
For eight years, Dr. Jon Barrett, director of the Women & Babies Research Program at Sunnybrook Research Institute, led the 25-country, 106-centre trial to determine which of vaginal birth or planned caesarean section is safest for twins. The long-awaited results were clear: vaginal birth is as safe as a planned C-section for twins delivered between 32 and 38 weeks of gestation when the pregnancy is otherwise uncomplicated and the first baby presents head down.
Evidence from Barrett’s trial has helped to promote the practice of vaginal twin delivery across the globe, including in Hong Kong, in a regional obstetric unit that delivers about 6,000 babies and 100 pairs of twins annually.
As reported in the International Journal of Gynecology & Obstetrics, obstetricians at Kwong Wah Hospital have seen a drop in vaginal twin delivery from 70% in 1993 to as low as 10% in 2008. Since then, however, the rate in the unit has rebounded to 40% in 2012, in part because of the unit’s research showing outcomes for twins delivered via C-section were not better than those delivered vaginally, which in turn led to a change in the unit’s practice.
This, coupled with the results of Barrett’s study, suggests the time to revisit the policy on how twins are delivered is now, concluded the researchers.
To the Bone

Photo: ©iStock.com/Spondylolithesis
Radiation therapy can help reduce pain and improve quality of life for patients with bone metastases, when cancer spreads from its original site to the bone. Repeat treatment is often required, but data on the best dose are lacking.
Dr. Edward Chow, a senior scientist in the Odette Cancer Research Program at Sunnybrook Research Institute, led a study that compared two radiation doses in patients with painful bone metastases who required repeated treatment. It is the first such multicentre, randomized clinical trial to assess two radiotherapy doses and measure pain-relief scores.
The study spanned nine countries, including Canada. It enrolled 850 patients who had previously received radiation therapy and randomly assigned them to receive either 8 Gy in a single dose of radiation or 20 Gy in multiple doses. (Gy is short form for “gray unit,” which is used to measure the amount of radiation absorbed.)
Chow found that 48% of all patients who received their assigned treatment had less pain at the site of repeat radiation, as well as less need for pain-relief medication. The results also suggested that a single dose with 8 Gy might be preferable to 20 Gy administered in multiple doses because of similar pain relief and lower toxicity.
The findings, published in The Lancet, will help inform practice, policies and future research in treating patients with bone metastases.
The Cancer’s Been Treated. Now What?

Photo: ©iStock.com/abluecup
Cancer therapies have improved survival, but many patients experience pain and problems with mobility and functioning after treatment. To address these challenges, Dr. Sara McEwen, a scientist in the St. John’s Rehab Research Program at Sunnybrook Research Institute, co-authored a systematic review of rehabilitation interventions after treatment.
McEwen and colleagues identified areas that could be addressed by rehabilitation, including physical and cognitive functioning, fatigue, pain, depression, employment and nutrition.
The researchers observed that studies in this area are mainly on psychosocial oncology services and supportive care, which have had limited effectiveness for rehab outcomes. They noted fatigue is a major area of study and treatment, but the related issues of physical deconditioning and cardiorespiratory impairment have not been examined. Other areas that might benefit from attention to physical rehab include nutrition and energy conservation techniques for people with fatigue, said the researchers.
They also found an exception to the limitations in the literature: rehab after breast cancer. These studies, which have been done by physiotherapy researchers, have resulted in prevention and intervention guidelines for mobility, pain, swelling and function. On the back of this research, new rehabilitation knowledge and care for people with other types of cancer could follow.
Snapshot of an Outbreak

Illustration: Dr. Rob Fowler spent weeks looking after patients at the World Health Organization Ebola isolation facility in Conakry, Guinea. Photo: Courtesy of Dr. Rob Fowler
The 2014 Ebola outbreak began in a remote area in Guinea, in West Africa. It spread to the capital, Conakry, and to bordering countries Liberia and Sierra Leone. Although at press time the epidemic was ebbing, the damage wrought has been catastrophic. It is by far the largest Ebola outbreak ever. It has infected close to 25,000 people and killed more than 10,000 people.
Dr. Rob Fowler, a senior scientist in the Tory Trauma Research Program at Sunnybrook Research Institute, led a retrospective observational study of patients with Ebola virus disease (EVD) in Conakry from March 25 to April 26, 2014. The study, the first to describe patients’ demographic and clinical characteristics at the onset of the outbreak, was published in the New England Journal of Medicine.
The primary outcome was death. During the study period, 37 patients had lab-confirmed EVD; 24 were men and 14 were health care workers. On average, patients presented to hospital five days after the onset of symptoms, which were fever, fatigue, diarrhea and fast heart rate. All patients were treated with antibiotics; 76% were given intravenous fluids for dehydration.
The mortality rate was 43%, which is lower than that of past EVD outbreaks. The lower rate could be due to adherence to new guidelines that promote interventions, including use of fluid and electrolyte replacement, certain antibiotics and targeted lab testing, said the researchers. These findings highlight the need for rapid support for infection control practices to protect patients and health care workers.
While You Were Sleeping

Illustration: ©iStock.com/SisterSarah
Memory loss commonly affects more than one-third of patients who undergo general anesthesia for surgery. The effect can be lasting, especially in elderly patients, and is linked to poor outcomes and sometimes death.
Dr. Beverley Orser, an affiliate scientist in the Hurvitz Brain Sciences Research Program at Sunnybrook Research Institute and an anesthesiologist at Sunnybrook, and colleagues used a mouse model to look at why anesthetics can cause cognitive impairment. The study was published in The Journal of Clinical Investigation.
They found that memory loss receptors remain highly active long after the drugs have left the patient’s body, and that this activity can persist for days or months. The results suggest sudden memory loss after surgery can diminish a patient’s ability to think clearly at a time when loss of sleep and medications can also affect mental function, said Orser.
Age, health, and the type of surgery and anesthetic can also contribute to the likelihood of a patient experiencing memory loss, noted the researchers, who concluded the study with a call for more research.
On the Couch: Wills in Suicide Notes
Illustration: ©iStock.com/KIVILCIM PINAR
Suicide accounts for about one million deaths annually. To understand the mindset of people who commit suicide, some researchers have focused on the language and themes in suicide notes.
Drs. Mark Sinyor and Ken Shulman, clinician-scientists in the Hurvitz Brain Sciences Research Program at Sunnybrook Research Institute, took a different approach—analyzing who left wills in suicide notes.
They studied records of 1,565 deaths ruled as suicide that occurred in Toronto between 2003 and 2009. Among these, 285 suicide notes were left behind.
Within these notes, 59 had wills. Compared with those who left no note, or a note and no will, people who left wills were more likely to be single and live alone, and be divorced or widowed.
A major mood or psychotic disorder was detected in 73% of people who left a will, but none had dementia. This is the first study to examine will content in suicide notes. The researchers concluded that the high rate of mental illness around time of death is important for understanding the psychology of people who die by suicide and has legal implications for their ability to leave a valid will.
Penetrating Into Deep-Brain Territory
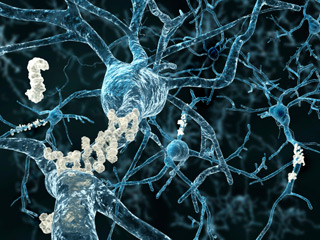
Illustration: ©iStock.com/selvanegra
Scientists at Sunnybrook Research Institute (SRI) are pioneering a noninvasive approach to treating Alzheimer’s disease and other brain disorders. At its essence, transcranial focused ultrasound increases the permeability of the blood-brain barrier temporarily such that antibodies and other therapeutic substances can slip through, directly to the source of the problem.
Recently, Dr. Kullervo Hynynen, director of Physical Sciences at SRI, and Dr. Isabelle Aubert, senior scientist in Biological Sciences at SRI, co-authored a study to examine whether repeated magnetic resonance imaging (MRI)-guided focused ultrasound treatments targeted to the hippocampus, a structure involved in memory and spatial navigation, could change pathological abnormalities, plasticity and behaviour.
The researchers used MRI-guided focused ultrasound to treat the hippocampus weekly in a mouse model of Alzheimer’s disease. One month later, they assessed changes.
They found that repeated MRI-guided focused ultrasound targeted to the hippocampus improved spatial memory in the treated mice, which they suggest might have been the result of reduced plaque load and increased neuronal plasticity due to the treatment. Indeed, the mice performed as well as those that didn’t have Alzheimer’s disease. Moreover, the hippocampus of treated mice had more newborn neurons and longer, more branched dendrites.
Published in Radiology, the study shows the therapy has the potential to ameliorate symptoms and abnormalities associated with Alzheimer’s disease, and improve drug delivery to the brain.
Arresting Stroke

Illustration: ©iStock.com/Planet Flem
Scientists at Sunnybrook Research Institute were part of an international clinical trial that showed rapid endovascular treatment, a procedure used to remove blood clots in the brain, can reduce the death rate by 50% and decrease neurological disability in patients who experience a moderate to severe ischemic stroke. So compelling were interim findings that the study was stopped early. Dr. Richard Swartz, a scientist in the Hurvitz Brain Sciences Research Program, was an investigator on the trial.
Endovascular treatment is a minimally invasive procedure that involves inserting a catheter into the artery in the groin, through the body and into the brain vessels to the clot. Under X-ray image guidance the clot is pulled out by a retrievable stent, thereby restoring blood flow to the brain.
The study, led by the University of Calgary and published in the New England Journal of Medicine, enrolled 316 patients from 22 sites who arrived at hospital within 12 hours of their stroke. Patients were randomized to receive either standard care with a clot-busting drug or the clot-busting drug plus rapid endovascular treatment. After 90 days, patients who received endovascular treatment had better outcomes—they went home after treatment and did not experience major neurological disability—and fewer of them died: 10% versus 19% of those who did not receive the intervention.
“This is the most significant advance in emergency stroke treatment in the last 20 years, and Canada will be one of the first countries to incorporate this treatment into stroke best practice guidelines,” said Swartz.



