Major study finds convalescent plasma doesn’t help seriously ill COVID-19 patients
A major study has found that convalescent plasma does not reduce the risk of intubation or death for COVID-19 patients. However, the study also revealed that the antibody profile in the blood of people who have had the virus is extremely variable and this may modify the response to the treatment.
Results of the international multi-centre study, led by researchers at Sunnybrook, McMaster University and CHU Sainte-Justine, were published in the journal Nature Medicine today.
“It has been thought that the blood plasma of COVID-19 survivors would help those seriously ill from the virus but, unfortunately, it does not,” said Dr. Donald Arnold, co-principal investigator of the study, hematologist and professor of medicine at McMaster University.
“We are cautioning against using convalescent plasma to treat COVID-19 hospitalized patients, unless they are in a closely-monitored clinical trial.”
The Canadian-led international research team also found that patients receiving convalescent plasma experienced significantly more serious adverse events than those receiving standard care. The majority of those events were an increased need for oxygen and worsening respiratory failure. However, the rate of fatal incidents was not significantly different from the control group of patients who did not receive the blood.
The clinical trial, called CONCOR-1, stopped enrolment early in January 2021 after its independent data safety monitoring committee recommended the study was unlikely to demonstrate a benefit of convalescent plasma even if more patients were enrolled. The trial included 940 patients at 72 hospitals in Canada, the United States, and Brazil. The U.S. team was coordinated by Weill Cornell Medicine.
A secondary discovery was that convalescent plasma had highly variable donor antibody content due to the highly variable immunological response to the virus. Different antibody profiles in the convalescent plasma were observed to significantly impact whether or not patients experienced intubation or death. Unfavourable antibody profiles, meaning low antibody titres, non-functional antibodies or both, were associated with a higher risk of intubation or death.
“These findings may explain the apparent conflicting results between randomized trials showing no benefit, and observational studies showing better outcomes with higher titre products relative to low titre products,” said Dr. Jeannie Callum, co-principal investigator, associate scientist at Sunnybrook Research Institute, and professor at Queen’s University and the University of Toronto.
“It appears that it may not be that high-titre convalescent plasma is helpful, but rather that low-titre convalescent plasma is harmful.”
Co-principal investigator Dr. Philippe Bégin said that the harm may come from the transfusion of convalescent plasma containing poorly functioning antibodies.
“One hypothesis is that those dysfunctional antibodies could compete with the patient’s own antibodies and could disrupt the mounting immune response. This phenomenon has been observed previously in pre-clinical models and in human studies of HIV vaccines.”
Dr. Bégin is a clinician scientist at Center hospitalier de l'Université de Montréal (CHUM) and CHU Sainte-Justine and an associate professor of the University of Montréal.
He added that the CONCOR-1 investigators are expecting to collaborate with other international study investigators to understand potential risks and benefits of convalescent plasma.
“This information from Canada’s largest clinical trial on convalescent plasma and COVID-19 may be analyzed together with the results of several similar studies going on in the world to provide more robust information and insight that will guide clinical practice and health policy globally,” Dr. Bégin said.
CONCOR-1 was an open-label randomized controlled trial of convalescent plasma or standard of care for hospitalized adults with acute COVID-19 respiratory illness. The study excluded COVID-19 patients who did not need to be in the hospital, and COVID-19 hospital patients who needed intubation at the time they were admitted to the hospital.
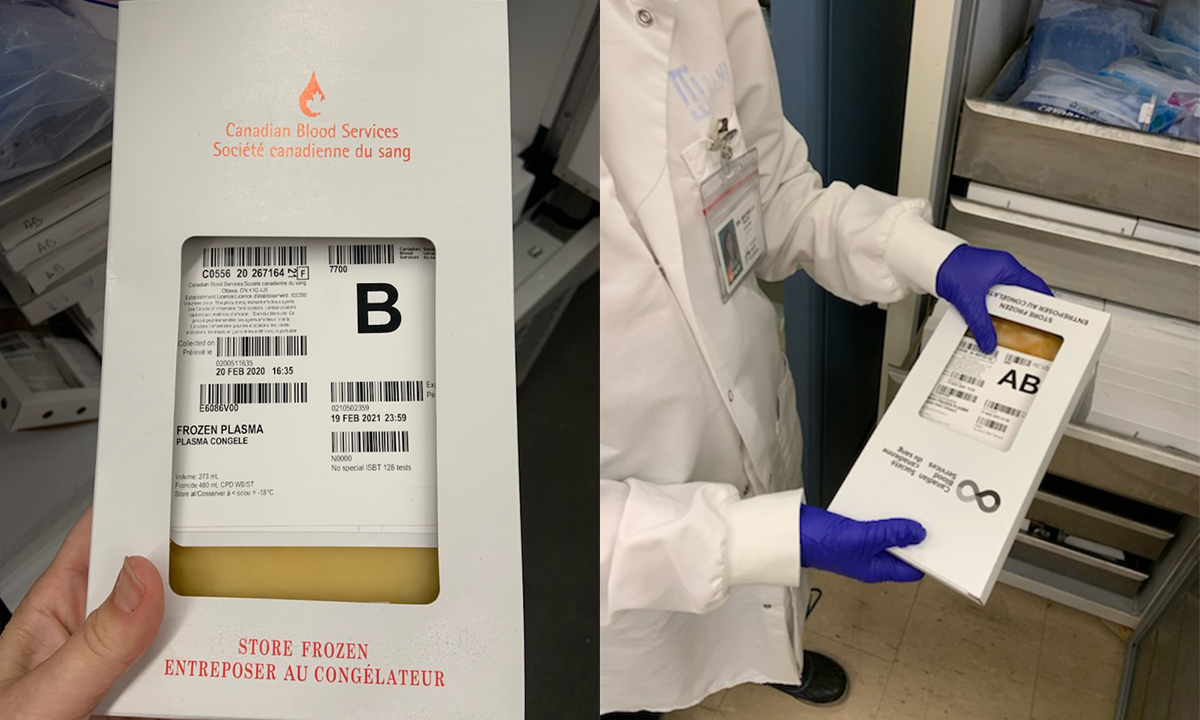
The $5.5 million trial was funded by the Canadian Institutes of Health Research, Canadian Blood Services, Héma-Québec, Sunnybrook Foundation, Ontario Research Fund, Quebec Ministry of Economics and Innovation, the University of Toronto, the Government of Saskatchewan Ministry of Health, Sunnybrook Health Sciences Centre, University Health Network, McMaster University, University Health Foundation at University of Alberta Hospital, Sinai Health System Foundation, CHU Ste. Justine Foundation, the Ottawa Hospital Academic Medical Organization, the Ottawa Hospital Foundation COVID-19 Research Fund and numerous generous private donors.
Media contacts:
Veronica McGuire
Media Relations
Faculty of Health Sciences
McMaster University
289-776-6952
vmcguir@mcmaster.ca
Samantha Sexton
Communications Advisor
Sunnybrook Health Sciences Centre
samantha.sexton@sunnybrook.ca
Justine Mondoux-Turcotte
Media Relations
CHU Sainte-Justine
514-213-4488
justine.mondoux.turcotte.hsj@ssss.gouv.qc.ca
Jen Gundersen
Assistant Director of Media Relations
Cornell University
917-242-2389
jeg2034@med.cornell.edu