Management
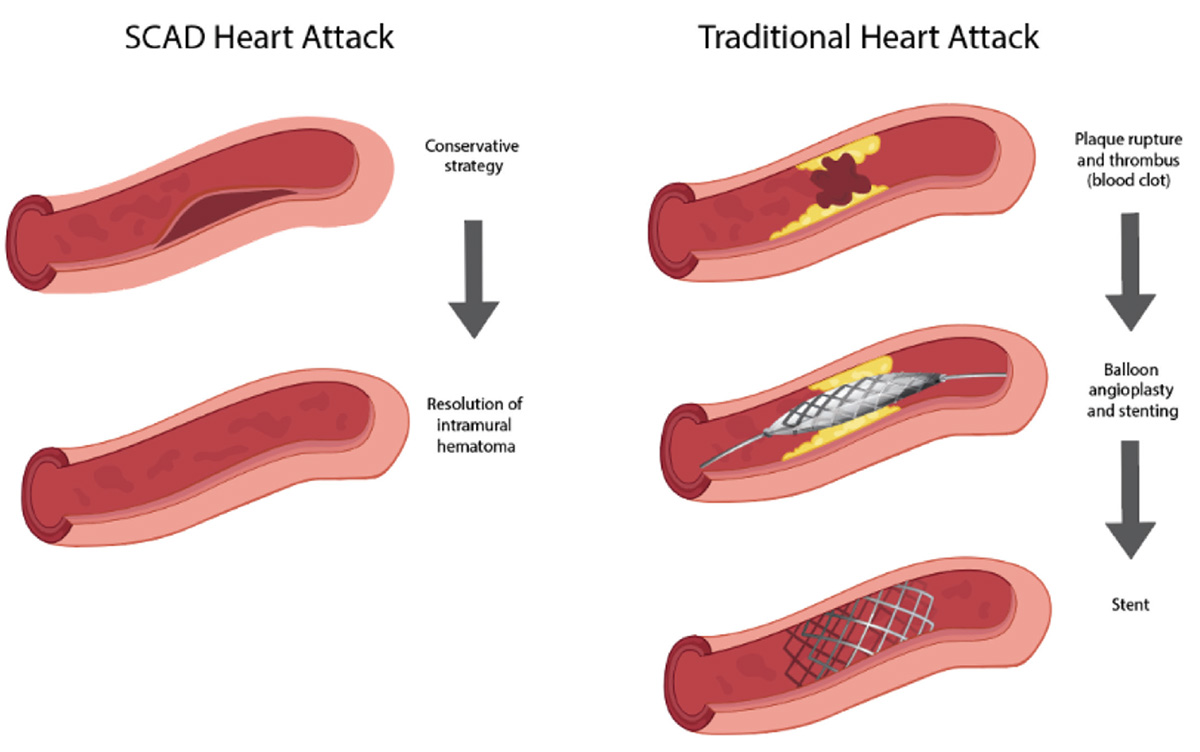
Unlike traditional heart attacks which do not get better on their own, the majority of SCAD blood vessels heal with no treatment. Studies which looked at SCAD blood vessels with a repeat coronary angiogram 30 days after the first SCAD heart attack, showed that 95% of SCAD blood vessels had healed without treatment. This is why we don’t treat most SCAD related heart attacks with invasive therapies.
Although a conservative strategy is used for the majority of patients, 2-8% of patients need invasive treatment because the tear and blood build up in the affected blood vessel does not resolve on its own or gets worse.
A few patients who do not improve without treatment or have severe SCAD heart attacks, need to have the blockage of the coronary artery fixed. This process is known as revascularization. Options for revascularization include percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG).
Percutaneous Coronary Intervention (PCI)
Percutaneous coronary intervention (PCI) may be considered in patients who have a SCAD heart attack with unstable features (ongoing chest pain, unstable condition, very large heart attack) or multiple coronary arteries affected by SCAD.
In these situations, the goal of PCI is to restore blood flow to the blocked SCAD blood vessel to minimize the damage to the heart. PCI uses a balloon to open the blockage in the coronary artery and possibly place a stent afterwards to keep the artery open. If needed, PCI can be performed immediately after the coronary angiogram is completed.
PCI is usually a lifesaving intervention in SCAD heart attacks. Some complications of PCI include recurrent coronary artery blockages in the stent, incorrect stent size for the blood vessel and residual blockages despite stent placement. Patients who require PCI for a SCAD heart attack have a higher risk of requiring a repeat procedure for recurrent coronary artery blockages compared to patients who can be managed with a conservative strategy.
Coronary Artery Bypass Grafting (CABG)
Coronary artery bypass grafting (CABG) is heart surgery to restore blood flow to a blocked coronary artery. It takes a blood vessel from another part of the body (usually chest wall or leg) and attaches it to the coronary artery above and below the blockage to bypass it. This new blood vessel is known as a graft. The number of grafts you will need is dependent on the number of blockages that need to be bypassed. This procedure is performed under general anesthesia, which means you will be unconscious during the operation.
A very small minority of patients with SCAD heart attacks undergo heart surgery. Patients would be considered for CABG if they have a life-threatening SCAD heart attack and PCI is not possible. Most patients who undergo CABG do well in the long term, with the highest risk occurring in the immediate period surrounding the surgery. In the long term, it is common for these grafts to become blocked in more than 60% of cases as the patient’s SCAD blood vessel heals and the grafts are no longer required to redirect blood flow. Although graft closure is a long-term risk, the initial CABG operation is usually lifesaving.
Figure 2: Management of SCAD heart attacks compared with traditional heart attacks.