Taking care of yourself after birth
Your nurse will be checking on your condition every 4 hours for the first 24 hours, or every hour if you've had a caesarean. After that, they will be checking you twice a day or as necessary.
Below are some suggestions & information that can help you during your recovery from labour and delivery.
Getting up
Please call your nurse the first time you wish to get out of bed. It is important to have your nurse there as many women often feel faint the first time they get up.
Your uterus
Gradually over the next few weeks your uterus will contract (shrink) back to its normal size and position. After delivery you can feel it just under your belly button and it's about the size of a grapefruit. It takes about six weeks to go back to its normal size.
Oxytocin is a hormone that your body makes and helps your uterus contract.

Afterpains
Afterpains are caused from your uterus contracting and cramping after birth. While afterpains keep your uterus firm and decrease bleeding, they can be very uncomfortable. Afterpains are particularly noticeable in the first 2-3 days after birth and tend to be worse with each pregnancy. They are more noticeable and increase in discomfort when you are breastfeeding.
To ease the discomfort of afterpains, try:
- Relaxation breathing techniques that you used while in labour.
- Walking slowly after delivery.
- Keeping your bladder empty.
- Use the medication in the self medication pack before breastfeeding and activity such as walking.
Vaginal discharge
After delivery, the contraction of your uterus removes extra blood and tissue. This continues for 2 to 6 weeks after birth.
The first day after delivery, bleeding can be heavy and bright to dark red in colour. Let your nurse know if you have any blood clots that are larger than a dollar coin.
A slight increase in bleeding is normal with a full bladder, during increased activity, and while breastfeeding.
Vaginal tear/episiotomy
As your baby is born, your perineum, the area between your vagina and rectum, stretches and sometimes tears. If the tear is small you may experience swelling, bruising and stinging. If the tear is large you will have had stitches and may experience increased pain.
Sometimes, an episiotomy is done. This is a small cut that makes more room for your baby to be born and requires stitches.
Stitches will dissolve on their own over the next 4-6 weeks.
Tips on taking care of your perineum
- Take your pain medication.
- Each time you use the toilet, rinse your perineum with warm water using your plastic bottle.
- Pat dry with toilet paper from front to back.
- When urinating, use the plastic bottle to spray water over your perineum to decrease stinging / pain.
- Change your pad every time you use the toilet.
- Use ice packs on your perineum, on and off as needed, for comfort and to lessen swelling.
- Your nurse can show you where to get ice.
Taking care of your perineum can help you feel more comfortable, help healing and prevent infection.
Bladder care

Urinating can be difficult because of pain and swelling and sometimes you might have a difficult time controlling the flow.
- Use the plastic bottle to spray on your perineum to help you urinate.
- Try to empty your bladder at least every 3 hours.
- Drink when you are thirsty.
- Sit comfortably on the toilet.
- Urinating a lot in the first week after your baby is born is normal.
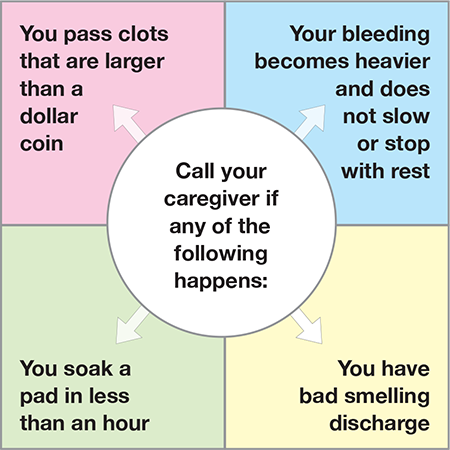
Call your caregiver if any of the following happen:
- You can't urinate.
- You have burning when urinating.
- You are urinating often and only a little at a time.
These signs, as well as fever, can mean you have an infection.
Bowel movements
You should have a bowel movement (BM) within 4 days after the birth of your baby. It may be difficult to have a bowel movement because of pain and bruising from your stitches.
Tips to reduce constipation:
- Drink when you are thirsty, about 6-8 glasses a day.
- Walk and do some light exercise.
- Eat fresh vegetables, fruit and whole grains.
- Take medication for relief of constipation.
- Support your perineum with toilet paper to provide some support.
Hemorrhoids
You may have hemorrhoids which are swollen veins around the rectum. They can be sore from pushing out your baby.
Tips for comfort and healing:
- Use ice packs on and off for the first 24 hours.
- Don't sit for a long time.
- Lie on your side.
- Keep your stools soft (see tips above).
- Ask you caregiver for hemorrhoid medication if needed.
Cramps
Cramps are normal and happen because your uterus is getting smaller. They keep your uterus firm and lessen the bleeding, but can be painful. You may feel cramps more in the first 2-3 days and you may feel them more if this is not your first baby and while breastfeeding.
Tips for pain:
- Take your pain medication regularly.
- Urinate at least every 2-3 hours.
- To help you relax, try taking slow deep breaths.
Sitz baths
A sitz bath is a portable basin that rests in the toilet bowl. It allows you to bathe your stitches and hemorrhoids with warm water. The bath helps to clean, heal, and soothe your stitches.
Sitz baths can be purchased from the hospital gift shop.
Self medication package
Managing your pain has many benefits. Pain relief helps your body heal, quickens your recovery, helps you relax and increases your comfort while breastfeeding.
You will be provided with a self-medication package containing ibuprofen (also known as Advil) and acetaminophen (also known as Tylenol). Both medications are used to relieve pain and are safe to use when breastfeeding.
Ibuprofen is especially helpful for pain related to inflammation (swelling), which is common after delivery or surgery. Acetaminophen is a pain reliever.
Although they work differently, they can be used together with the goal of providing better pain relief.
Your nurse will explain the contents of the self-medication package and its use.
Birth control after baby is born
Please visit Toronto Public Health (see tab “Contraception, Birth Control”) for more details about how breastfeeding can be effective in preventing pregnancy.
At home: is this normal?
Below are some tips and information to help you know what's normal and when to get help after being home with baby.
You are doing well if:
- Your vaginal bleeding is decreasing in amount by day 3 to 5.
- Your pain is controlled by over-the-counter pain medication.
- You are gradually resuming your routine activities.
- Your fundus is firm.
- Your bladder feels empty after peeing. Peeing is not painful.
- You have a bowel movement by day 2 to 3 (vaginal birth) or day 3 to 5 (caesarean birth).
- Your caesarean section incision, episiotomy, or tear is healing.
- Your breasts are soft (day 1 to 2) and filling (day 3 to 4).
- You are able to sleep or rest between baby's feedings.
When to get help for mother:
Call your doctor right away if:
- You pass many clots that are larger than a "plum" and your vaginal bleeding becomes heavier and does not slow or stop with rest.
- You have bright red blood after ten days.
- You have foul smelling vaginal discharge.
- You have painful, swollen lower legs.
- You have pain when you pee. You feel burning every time you pee. You find it hard to pee.
- You have pain that is not relieved by over-the-counter pain medications.
- You feel feverish with flu like symptoms or your temperature is over 38°C.
- You see changes in your caesarean section incision, episiotomy, or tear. You see redness or discharge coming from the incision.
- You have a headache, or blurred vision or heartburn that is not improving.
If you cannot reach your doctor and any of the above situations is not getting better, please go to your nearest walk-in clinic or hospital emergency.
Call 911 or go to the nearest emergency department IMMEDIATELY if:
- You have heavy vaginal bleeding that completely soaks one or more sanitary pads in 2 hours and does not slow or stop at rest.
- You have trouble breathing or chest pain, severe headache, heartburn, blurred vision.