The day of surgery
» For patients having a mastectomy and an axillary lymph node dissection
![]() Please bring a paper copy of this guide with you on the day of your surgery.
Please bring a paper copy of this guide with you on the day of your surgery.
Registration
Where do I check in?
- When you get to the hospital, check in at the Surgical Services Registration Desk. It is in M Wing, Ground Floor, Room 502 (MG 502).
- Bring your Ontario Health Card.
- You will be given a locker space to store your clothes and personal items, such as eye glasses, during your surgery.
Please do not bring:
- Money
- Jewelry
Please label with your name and contact information:
- Cell phones
- iPads or other electronic devices
The hospital will not take responsibility if they are lost or stolen.
How many family members or friends can come with me on the day of surgery?
- Please bring ONLY 1 person with you to the hospital. Your companion will be asked to stay in the waiting room until you are ready for surgery. The person can then be with you until you are called for surgery.
- During your surgery, your family member or friend can wait in room MG 502.
 Note:
Note:
Very rarely, surgery cases are cancelled because there is someone else who needs an emergency surgery. If this happens to you, you will be contacted by your surgeon’s office and a new surgery date will be booked as soon as possible.
Operating room
Once you have completed registration, you will be taken to the Same Day Surgery Unit. Nurses will complete the final checks and an intravenous (IV) will be started in your hand. When the surgeon is ready, you will be brought into the operating room.
What will happen during my surgery?
- You will be put to sleep using a general anesthetic. Medication to make you sleep will be given through an intravenous needle.
- A tube will be placed in your throat to help you breathe when you are asleep.
- A cut (incision) is made and the whole breast is removed. All of the lymph nodes will also be removed from the armpit area.
- All the tissue that is taken out will be sent to a lab to be examined by a pathologist (a doctor).
- The number of lymph nodes removed and if there is any cancer in them, is not known until the final results are completed. It can take two to three weeks for this information to be available.
- One or more drainage tubes are put in place to drain the fluid from the area.
- The cut area (incision) is closed with stitches that dissolve and covered with paper tapes (known as Steri-Strips). A dressing, or bandage, is placed over the skin tapes.
After surgery
What will happen after the operation is done?
- After your surgery is done, you will be taken to the Post Anaesthetic Care Unit (PACU), which is also known as the recovery room.
- When you are awake you will be moved back to the Same Day Surgery Unit in Room MG 601.
- Most patients go home the same day as surgery.
- There will be 1 or 2 drains in place. Instructions on how to care for your drain will have been explained to you in a pre-surgery class. Before you go home, your nurse will review the instructions with you.
- A nurse will call your family member or friend to come visit you.
- The surgery team will give you a prescription for pain medication before you leave the hospital.
- Nursing care will have been arranged for you by your surgeon’s office to help you with your drain care either in your home or at a community clinic.
- You will continue to rest and recover. The nurses will start to get you ready to go home.
- One of the nurses from the cancer centre will call you the next business day after your surgery.
- If you are staying in the hospital overnight, the occupational therapist, physiotherapist and surgical team will see you in the morning. The nurse will review with you the drain instructions.
What are the things I need to do after my surgery?

Deep breathing and coughing:
- Do deep breathing exercises as soon as possible to keep your lungs clear after surgery.
- Do 10 deep breaths four to five times during the day while you are awake for the first 48 hours after surgery.
- Try and cough two to three times after you do your deep breathing.
- Coughing up a bit of sputum (thick mucus or phlegm) after surgery is common.
Movement:
- You should move your arm(s) soon after your surgery.
- DO NOT cradle your arm(s) against your chest.
» For patients having a mastectomy and sentinel lymph node biopsy
![]() Please bring a paper copy of this guide with you on the day of your surgery. Before you go into the operating room, you will need to complete 2 steps:
Please bring a paper copy of this guide with you on the day of your surgery. Before you go into the operating room, you will need to complete 2 steps:
- Registration
- Sentinel lymph node injection appointment
Registration
Where do I check in?
- When you get to the hospital, check in at the Surgical Services Registration Desk. It is in M Wing, Ground Floor, Room 502 (MG 502).
- Bring your Ontario Health Card.
- You will be given a locker space to store your clothes and personal items, such as eye glasses, during your surgery.
Please do not bring:
- Money
- Jewelry
Please label with your name and contact information:
- Cell phones
- iPads or other electronic devices
The hospital will not take responsibility if they are lost or stolen.
How many family members or friends can come with me on the day of surgery?
- Please bring ONLY 1 person with you to the hospital. Your companion will be asked to stay in the waiting room until you are ready for surgery. The person can then be with you until you are called for surgery.
- During your surgery, your family member or friend can wait in room MG 502.
 Note:
Note:
Very rarely, surgery cases are cancelled because there is someone else who needs an emergency surgery. If this happens to you, you will be contacted by your surgeon’s office and a new surgery date will be booked as soon as possible.
Sentinel Lymph Node Injection Appointment
As part of your mastectomy, the surgeon will remove sentinel lymph nodes in the armpit on the same side as the breast cancer. The lymph nodes need to be specially identified before your surgery. This identifi cation is called a Sentinel Lymph Node Injection. The injection takes place in the Department of Nuclear Medicine. The department is in A Wing, Ground Floor, Room 21 (AG 21). You will be given a map showing the location when you check in at the Surgical Services Registration Desk in M-Wing, Ground Floor, Room 502 (MG 502). The appointment can take up to an hour.
What happens during the sentinel lymph node injection?
- The sentinel nodes are specially identified so the surgeon can find them.
- This is done by injecting a small amount of radioactive tracer into the breast.
- The tracer travels to the sentinel lymph nodes.
- The amount of radiation that the tracer gives off is very little. It will not harm you.
How do I get ready for the injection?
- The injection is made into the skin near your nipple and may sting.
- You may want to use EMLA cream and/or Tylenol (acetaminophen) to help reduce any pain or discomfort.
- You can buy the EMLA cream at a pharmacy. You do not need a prescription.
- Put the cream outside the areola (the dark area of the nipple) on the breast needing surgery up to 1 hour before your appointment.
- You can take some Tylenol (acetaminophen) up to 30 minutes before the injection (DO NOT take Tylenol if you are allergic to it).
- Please DO NOT take Aspirin (acetylsalicylic acid or ASA) because it may increase bleeding from surgery.
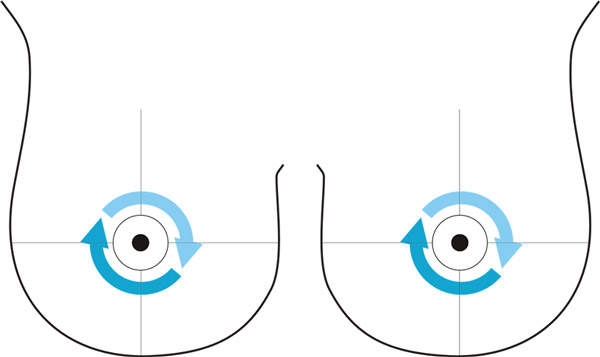
Apply EMLA cream to the breast needing surgery around the areola as shown by the arrows on the diagram.

Note:
Some patients have the sentinel lymph node injection appointment on the day before their mastectomy surgery. Your surgeon's office will confirm with you when your appointment will take place.- If you are one of these patients, go directly to the Department of Nuclear Medicine – in Room AG 21 – at your appointment time. Make sure you bring your Ontario Health Card and Sunnybrook Card.
- The appointment can take up to 1 hour. You will go home afterwards.
- The next day you will come back to the hospital for your mastectomy surgery and the removal of the sentinel lymph nodes.
- When you get to the hospital on the day of your surgery, please check in at the Surgical Services Registration Desk. It is located in M Wing, Ground Floor, Room 502 (MG 502).
Operating room
Once you have finished all your pre-surgery appointments, you will be taken to the Same Day Surgery Unit. Nurses will complete the final checks and an intravenous (IV) will be started in your hand. When the surgeon is ready, you will be brought into the operating room.
What will happen during my surgery?
- You will be put to sleep using a general anesthetic. Medication to make you sleep will be given through an intravenous needle.
- A tube will be placed in your throat to help you breathe when you are asleep.
- The surgeon may inject a blue dye into the breast as part of the sentinel lymph node biopsy. This is done after you are asleep. The dye travels to the nearby sentinel nodes and helps the surgeon see them more clearly.
- An incision (cut) is made and the whole breast and the nipple is removed.
- Some of the lymph nodes will also be removed.
- All the tissue that is taken out will be sent to a lab to be examined by a pathologist (a doctor).
- The number of lymph nodes removed and if there is any cancer in them, is not known until the final results are completed. It can take two to three weeks for this information to be available.
- One or two drainage tubes are put in place to drain the fluid from the area.
- The cut area (incision) is closed with stitches that dissolve and covered with paper tapes (known as Steri-Strips). A dressing, or bandage, is then placed over the skin tapes.
After surgery
What will happen after the operation is done?
- After your surgery is done, you will be taken to the Post Anesthetic Care Unit (PACU), which is also known as the recovery room.
- Most patients go home the same day.
- When you wake up, you will be moved back to the Same Day Surgery Unit in Room MG 601.
- There will be 1 or 2 drains in place. Instructions on how to care for your drain will have been explained to you in a pre-surgery class.
- A nurse will call your family member or friend to come visit you.
- The surgery team will give you a prescription for pain medication before you leave the hospital.
- Nursing care will have been arranged for you by your surgeon’s office to help you with your drain care either in your home or at a community clinic.
- You will continue to rest and recover. The nurses will start to get you ready to go home.
- One of the nurses from the cancer centre will call you the next business day after your surgery.
- If you are staying in the hospital overnight, the physiotherapist, occupational therapist and the surgical team will see you the next morning. The nurse will review drain instructions with you.
What are the things I need to do after my surgery?

Deep breathing and coughing:
- Do deep breathing exercises as soon as possible to keep your lungs clear after surgery.
- Do 10 deep breaths four to five times during the day while you are awake for the first 48 hours after surgery.
- Try and cough two to three times after you do your deep breathing.
- Coughing up a bit of sputum (thick mucus or phlegm) after surgery is common.
Movement:
- You should move your arm(s) soon after your surgery.
- DO NOT cradle your arm(s) against your chest.






