Home hemodialysis
Overview
How hemodialysis (HD) works
- Hemodialysis cleans the blood through a hemodialysis machine and filter (dialyzer)
- Access to bloodstream is required and is usually created ahead of time in arm or chest
-
Performed by individual or caregiver at home
-
Can be done during the day (conventional or short daily hemodialysis) or during the night (nocturnal hemodialysis)
-
Plumbing and electrical modifications are required prior to machine installation
-
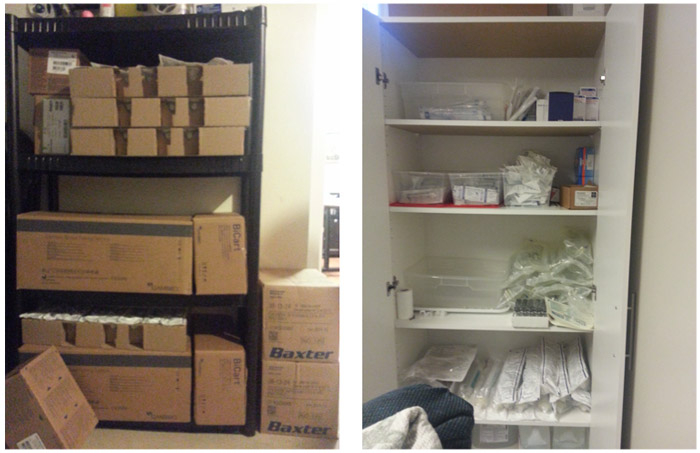
Space is required for supplies
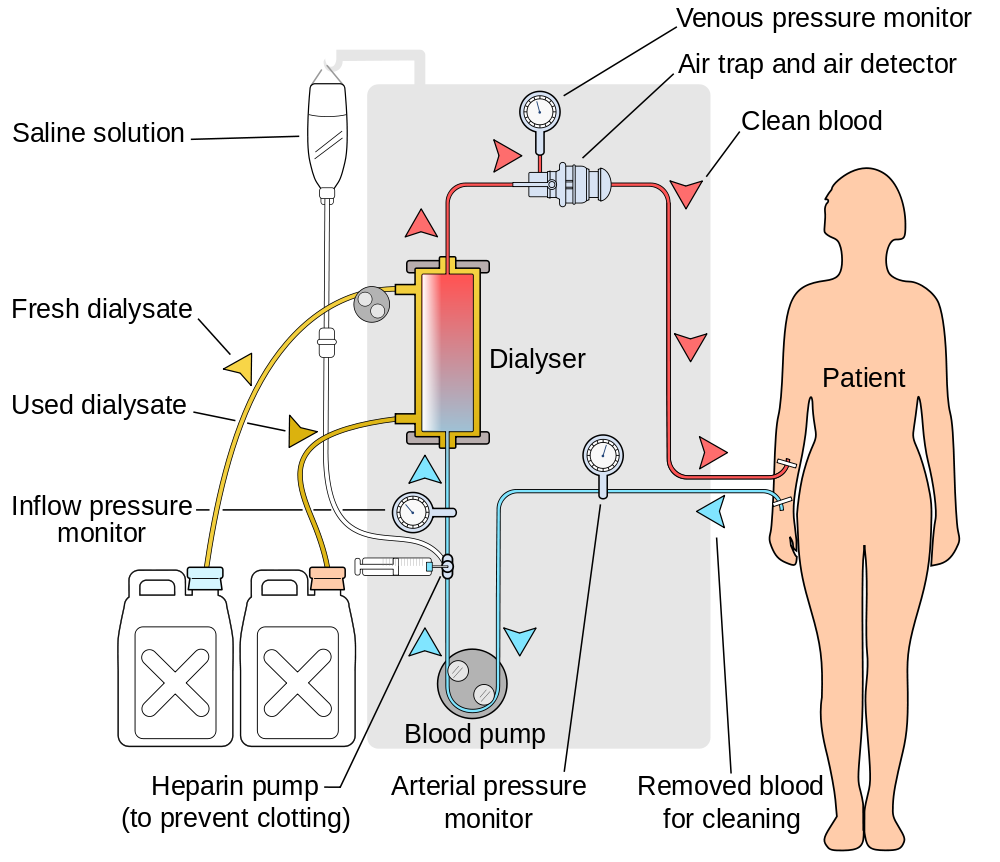
Image created by YassineMrabet - Creative Commons license (CC BY 3.0)
Home HD machine
Home HD water treatment system

Training and support
- Home dialysis nurses provide training for home hemodialysis that may take 6-8 weeks
- Home dialysis nurses and technical support are on-call 24/7
- Routine home visits and telephone calls from home dialysis team
- Clinic visits with your kidney team occur every 1-2 months
- Home care nurses (CCAC) are not available to provide home hemodialysis
Why might I consider home hemodialysis?
- Travel is possible, but requires arrangements
- Flexibility of time/schedule
- Avoids frequent travel to a dialysis unit
- May improve/benefit individual medically
- Decreased impact on work/life/social activities
What are common risks on home hemodialysis?
- Infection: central venous catheters are associated with the highest risk of bloodstream infections which may result in a serious infection requiring hospitalization
- 1 in 5 chance of developing a bloodstream infection
- Low blood pressure: may occur as a result of fluid removal during dialysis and rarely can result in loss of consciousness
- Blood loss: can occur as a result of clotting in tubing, bleeding from access sites, accidental disconnection from machine
Learn more
1. Hemodialyis: the basics
Our interprofessional team
- Our home dialysis team includes a nephrologist (kidney doctor), nurses, dialysis access coordinator, dietitian, social worker, pharmacist, patient care manager, technologist, and patient administrative assistant
- We work together to manage the health care needs of individuals on dialysis
Types of dialysis
There are two types of dialysis:
- Peritoneal dialysis (PD) = Belly dialysis
- Hemodialysis (HD) = Blood dialysis
Our team works with individuals to determine the type of dialysis that is most suitable for them.
How hemodialysis works
- Hemodialysis means “cleaning the blood”
- Blood is taken from the body by a hemodialysis machine, passed through a dialyzer (artificial kidney), and returned back to the body
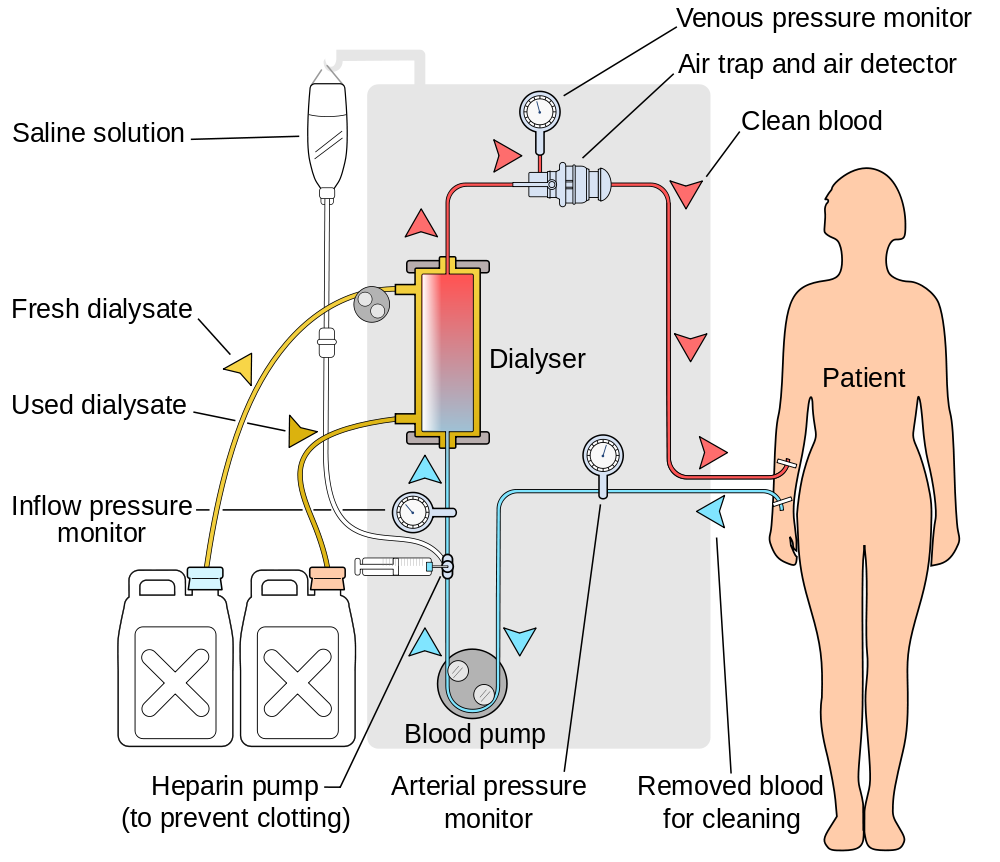
Image created by YassineMrabet - Creative Commons license (CC BY 3.0)
Vascular access for hemodialysis
- During hemodialysis blood is removed and returned via the vascular access.
- The vascular access is put in place or created before an individual needs hemodialysis.
- The vascular access is usually placed in the arm or chest, but can also be placed in the neck or leg.
- All forms of vascular access need ongoing care and occasional procedures to make sure that they continue to work.
Vascular Access Clinic
In preparation for hemodialysis individuals will be referred to the Vascular Access Clinic where they will:
- be assessed for creation of a vascular access
- have an ultrasound of both arms to assess the size and quality of veins
- meet with the vascular surgeon, dialysis access coordinator and a nephrologist to discuss options
2. Hemodialysis: the settings
1. In-centre (hospital) – Nurses perform dialysis
2. Community-based facilities:
- Sheppard Centre – Nurses and patients perform dialysis together
- Dialysis Management Clinic (DMC) – Nurses perform dialysis
3. Homes – Patients, caregivers and/or family members perform dialysis
Hemodialysis treatments
1. In-centre & community-based hemodialysis
- Three sessions per week
- Each session is four hours in duration
- Individuals assigned to a fixed dialysis shift
- e.g. Monday, Wednesday & Friday mornings
2. Home hemodialysis
- Can deliver the same therapy as in-centre
- Can also deliver more dialysis as compared to in-centre, options include:
- Nocturnal (night time) dialysis
- Short daily dialysis
Why might I consider home hemodialysis?
Medical benefits
Individuals performing dialysis at home can receive MORE dialysis
- Nocturnal hemodialysis
- 4 – 6 nights per week
- 6 – 8 hours per session (during sleep)
- Short daily hemodialysis
- 5 – 6 days per week
- 2 – 2.5 hrs per session
Increasing the frequency of hemodialysis treatments beyond 3 times a week may improve some of the following:
- Blood pressure control
- Abnormal heart muscle thickening
- Blood phosphate levels (and possibly bone health)
- Fertility in women
- Sleep apnea
- Heart function
- Fluid removal tolerance
- Sexual function
Lifestyle benefits
- Flexible schedule
- Avoids travel to a dialysis unit
- May need fewer medications
Dietary benefits
- More dialysis can result in improvements in phosphate and fluid removal
- May allow a more liberal diet
3. Risks of home hemodialysis
Low blood pressure
- Removal of fluid during dialysis may cause a drop in blood pressure
- Risk of low blood pressure is less with nocturnal and short daily hemodialysis
- Limiting salt and water intake can help reduce this risk
- Muscle cramps may be associated with low blood pressure
- Although rare, very low blood pressure can result in loss of consciousness
Infection
- Bacterial contamination of the blood may result in serious infections, some requiring hospital admission
- Central venous catheters are associated with the highest risk of bloodstream infections
- 1 in 5 chance of developing a blood stream infection with a central venous catheter
- Careful vascular access selection and proper care can help reduce this risk
Blood loss
- Blood loss can occur as a result of:
- clotting in tubing
- bleeding from access sites
- accidental disconnection from machine
- Blood loss can require a medical intervention (e.g. blood transfusion)
- Leak detectors are used to alert individuals on nocturnal hemodialysis to an accidental disconnection
Vascular access
- Nocturnal and short daily hemodialysis are associated with more frequent vascular access procedures
4. Eligibility for home hemodialysis
Home hemodialysis assessment
- Requirements of individual
- Requirements of home
Individual and/or caregiver requirements
- Willingness and ability to learn hemodialysis at home
- Basic English reading and writing skills
- Ability to perform certain tasks easily by hand
- Adequate vision to operate equipment
Home requirements
- Clean and well lit room
- Space for water purification system, dialysis machine, reclining chair/bed, work table and storage of monthly supplies and increased garbage
- Telephone and backup lighting (flashlight)
- Consent from landlord for home modifications (if applicable)
- Larger garbage bins may be required (a letter to city can be provided)
At home

Storage space
Home installation
- May require electrical and plumbing modifications which will be arranged by the home dialysis team
- All modifications are performed by certified professionals and can be reversed
- Initial costs are covered by the home dialysis program
5. Education and support for home hemodialysis
Home hemodialysis education
- A medical background is not required
- Individualized education is provided by a home dialysis nurse in the unit
- Education sessions are typically held Monday through Friday between 7:30-3:30
- Each session takes approximately 4-5 hrs
- Approximately 6-8 weeks of education is required
- Free parking is provided during education sessions
Home hemodialysis supports
Clinic
- Visits to home hemodialysis clinic are generally required every month initially and then every 2 months
- In clinic individuals will be seen by interprofessional team
Nursing & home visits
- Individuals can call or make an appointment with home dialysis team during office hours
- Outside of regular office hours a home dialysis nurse is on-call
- Home visits will be provided
- Respite can be provided as needed
Technical support
- Available by phone at all times (including holidays and weekends)
- Monthly technologist home visits for water testing
- Regular home visits for preventative maintenance and repairs by technologist
6. Life on home hemodialysis
Daily routine on home hemodialysis
Self Assessment
- Weight
- Blood pressure
- Swelling
- HD access
Hemodialysis Treatment
- Setup
- Monitoring
- Disinfection
Finances
- Most individuals are able to continue working
- Water and electricity costs will increase
- Limited financial assistance may be available and some costs are tax deductible
Nutrition
- Some aspects of diet that may need to change include: protein, phosphorous, potassium, fluid and sodium
- Nutrition needs are unique for each individual and will be assessed by our dietitian. The dietitian will help in making food choices to meet those needs
- Each individual’s nutrition needs depend on many factors including: dialysis prescription, other illnesses, blood tests and the individual’s overall nutritional health
Medications
- When starting HHD, adjustments to the medication dose and timing may be needed as some are removed from the body through dialysis
- During training for HHD, a dialysis pharmacist will meet with individuals and their families to find the best times to take medications and to make sure they are appropriate
- While on HHD, some medications may be given through the dialysis machine. If this is required, our home dialysis team teaches individuals on how to give these medications
Travel
- Travel to many countries is possible
- Treatment arrangements need to be made 2-3 months before the planned trip
- The healthcare team will assist with arranging all testing and documents needed for travel
- OHIP provides full coverage for treatments within Canada and partial coverage for international treatments
Body image
Fistula or graft
- Fistula or graft is not visible above skin
- Lumps or scar tissue may be visible
- Past needle entry sites are often visible
Hemodialysis catheter
- A portion of the catheter remains outside the body
- Most catheter locations are typically covered by clothing
Lifestyle
- Individuals receiving hemodialysis may continue to work and participate in many physical activities or hobbies
- Swimming is permitted in individuals with a fistula or graft
Intimacy
- Individuals receiving hemodialysis may continue having an intimate relationship
- Kidney disease may affect sexual desires and/or activity
- Individuals who are interested in more information should talk to a member of the interprofessional team
Pregnancy
- Men and women on hemodialysis may be able to have children
- Conception in women on hemodialysis is less likely than in women with normal kidney function
- Nocturnal hemodialysis offers the best chance of both conceiving and having a healthy outcome for baby and mother
Relationships and mood
- Individuals may experience a wide range of emotions and are encouraged to speak with interprofessional team members
- Sharing experiences, feelings and concerns often helps strengthen personal relationships and resolve difficulties
- Peer support is available through the Kidney Foundation of Canada






