In-centre hemodialysis
Overview
How it works
- Typically 3 treatments per week in hospital
- Each treatment is approximately 4 hours, however, actual time required is about 5 hours
- Based on availability, an appointment time and schedule for treatments will be assigned
- Monday, Wednesday and Friday OR Tuesday, Thursday and Saturday 7:30 a.m., 12:30 p.m. or 5:30 p.m.
Treatment
- Continuous monitoring is provided by nursing staff
- Activity is restricted during treatment
- Eating before or after treatment is preferred, not during
- It may not be safe to drive if feeling unwell after treatment
- Travel is possible but requires arrangements
Support
- Monitoring is provided by the nursing staff of your kidney team
- Certain members of your kidney team will visit you weekly on dialysis
- If needed, you may request to see a member of your kidney team during one of your dialysis treatments
In-centre hemodialysis machine

Learn more
1. Hemodialysis: the basics
Our interprofessional team
- Our dialysis team includes nephrologists (kidney doctor), nurses, dialysis access coordinator, dietitians, social workers, pharmacists, patient care managers, technologists, clerical staff, support staff and volunteers
- We work together to manage the health care needs of individuals on dialysis
Types of dialysis
There are two types of dialysis:
- Peritoneal dialysis (PD) = Belly dialysis
- Hemodialysis (HD) = Blood dialysis
Our team works with individuals to determine the type of dialysis that is most suitable for them.
How HD works
Hemodialysis means “cleaning the blood”
Blood is taken from the body by a hemodialysis machine, passed through a dialyzer (artificial kidney), and returned back to the body
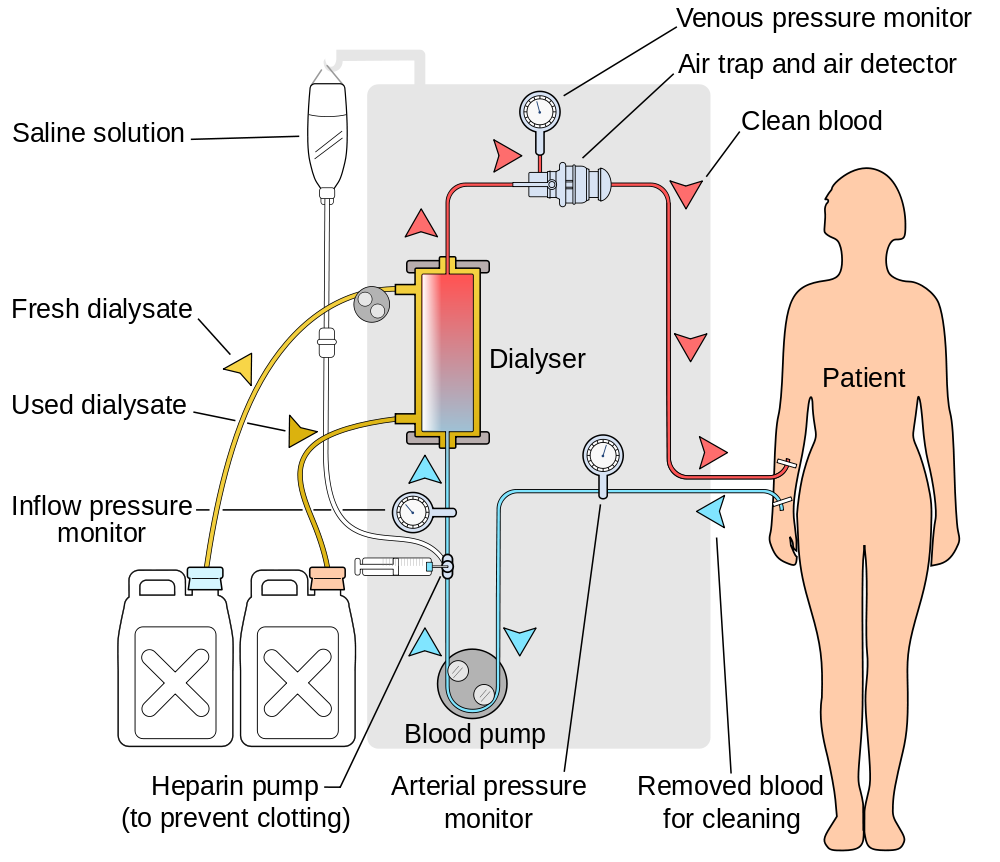
Image created by YassineMrabet - Creative Commons license (CC BY 3.0)
Vascular access for hemodialysis
During hemodialysis blood is removed and returned via the vascular access.
The vascular access is put in place or created before an individual needs hemodialysis.
The vascular access is usually placed in the arm or chest, but can also be placed in the neck or leg.
All forms of vascular access need ongoing care and occasional procedures to make sure that they continue to work.
Vascular Access Clinic
In preparation for hemodialysis individuals will be referred to the Vascular Access Clinic where they will:
- be assessed for creation of a vascular access
- have an ultrasound of both arms to assess the size and quality of veins
- meet with the vascular surgeon, dialysis access coordinator and a nephrologist to discuss options
2. Hemodialysis: the settings
1. In-centre (hospital) – Nurses perform dialysis
2. Community-based facilities:
- Sheppard Centre – Nurses and patients perform dialysis together
- Dialysis Management Clinic (DMC) – Nurses perform dialysis
3. Homes – Patients, caregivers and/or family members perform dialysis
In-centre hemodialysis
- Treatments performed at Sunnybrook by hemodialysis nurses
- Interprofessional team members available on site
- Individuals assigned to a hemodialysis shift
- Weekly rounds by nephrologist
Community-based facilities
- Individuals must meet eligibility criteria
- Treatments performed in a community facility by hemodialysis nurses
- Partial self care training may be required
- Interprofessional team members available by phone or at Sunnybrook
- Individuals assigned to a hemodialysis shift
- Clinic visits every 1-2 months at Sunnybrook
Why might I consider in-centre or community-based facilities?
- Limited training required
- Hemodialysis delivered by a health care professional
- Home environment free of hemodialysis supplies
3. Risks of in-centre hemodialysis
Low blood pressure
- Removal of fluid during dialysis may cause a drop in blood pressure
- Limiting salt and water intake can help reduce this risk
- Muscle cramps may be associated with a drop in blood pressure
- Although rare, very low blood pressure can result in loss of consciousness
Infection
- Bacterial contamination of the blood may result in serious infections, some requiring hospital admission
- Careful vascular access selection and proper care can help reduce this risk
- Central venous catheters have the highest risk of blood stream infection
- 1 in 5 lifetime risk of blood stream infection with central catheter usage
- Risk of hospital acquired infections
Blood loss
- Blood loss can occur as a result of:
- clotting in tubing
- bleeding from access sites
- accidental disconnection from machine
- Blood loss can require medical intervention (e.g. blood transfusion)
- Vigilant care is provided to prevent excess blood loss
4. In-centre hemodialysis unit procedures
Hemodialysis Unit
Hours of operations
- Monday to Saturday 7:30 a.m. - 10:30 p.m.
- Open all holidays except Christmas Day and New Year's Day
- Three shifts: morning (7:30 a.m.), afternoon (12:30 p.m.) and evening (5:30 p.m.)
Hemodialysis Schedules
Conventional
- 3 days per week
- Either Monday, Wednesday and Friday OR Tuesday, Thursday and Saturday
- 3.5 - 4 hours per session
Short Daily
- 5 – 6 days per week
- 2 – 2.5 hrs per session
Schedules
- Based on availability, an appointment time and schedule for treatments will be assigned
- Temporary or permanent schedule changes may be possible based on availability
Treatment environment
- Chairs & limited number of beds
- Television available for each patient
- One pillow and one blanket provided for each patient
Hemodialysis routine
- Before treatment
- During treatment
- After treatment
- Unit procedures
Before treatment
- Arrive 15 minutes ahead of time
- Use a hand sanitizer upon arrival
- Treatment location is found on large white board in hallway
- Wait in designated seating area to be called for treatment
- Vital signs and weight are assessed prior to treatment
During treatment
- Continuous monitoring throughout treatment is provided
- Activity will be restricted during treatment
- Watching television, listening to music, reading and other stationary activities are possible
- It is recommended to eat before or after treatment
After treatment
- Vital signs and weight are assessed
- Vascular access is observed for bleeding after needle removal
- Prolonged bleeding may delay departure
- It may not be safe to drive if feeling unwell
Unit procedures
Visitors
- Allowed once treatment is inittiated, but not during imitation and discontinuation
Parking
- Validation available for hemodialysis treatments only
Smoking
- Prohibited in all areas of the hospital
Electronic devices
- Computers, telephones chargers, and other devices may be used once checked to ensure they meet required standards
5. Life on in-centre hemodialysis
Nutrition
- Some aspects of diet that may need to change include: protein, phosphorous, potassium, fluid, and sodium
- Nutrition needs are unique for each individual and will be assessed by our dietitian, who will help in making food choices to meet those needs
- Each individual’s nutrition needs depend on many factors including: dialysis prescription, other illnesses, blood tests and overall nutritional health
Medications
- A pharmacist will review and discuss medications
- Adjustments to medication dose and timing may be needed as some are removed by hemodialysis
- Certain injectable medications such as Eprex®/Aranesp®, will be administered through the hemodialysis machine
Transportation
- Our team is available to help determine the most appropriate mode of transportation
- Individuals are responsible for transportation arrangements and costs
- Parking costs are only covered for hemodialysis treatments
- Individuals with mobility difficulties MAY be eligible for transportation services (i.e. Wheel Trans)
- In-person interview necessary to determine eligibility
- Community transportation services may be available for a fee
Travel
- Travel to many countries is possible
- Treatment arrangements need to be made 2-3 months before the planned trip
- The healthcare team will assist with arranging all testing and documents needed for travel
- OHIP provides full coverage for treatments within Canada and partial coverage for international treatments
Body image
Fistula or graft
- Created under the skin
- Lumps or scar tissue may be visible
- Past needle entry sites are often visible

- A portion of the catheter remains outside the body
- Most catheter locations are typically covered by clothing
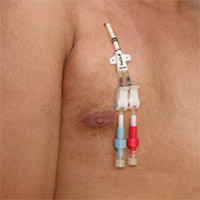
Image courtesy of The Kidney Foundation of Canada
Lifestyle
- Individuals receiving hemodialysis may continue to work and participate in many physical activities or hobbies
- Tax credits may be available
- Swimming is permitted in individuals with a fistula or graft
Intimacy
- Individuals receiving hemodialysis may continue having an intimate relationship
- Kidney disease may affect sexual desires and/or activity
- Individuals who are interested in more information should talk to a member of the interprofessional team
Pregnancy
- Men and women on hemodialysis may be able to have children
- Conception in women on hemodialysis is less likely than in women with normal kidney function
- Nocturnal hemodialysis offers the best chance of both conceiving and having a healthy outcome for baby and mother
Relationships and mood
- Individuals may experience a wide range of emotions and are encouraged to speak with interprofessional team members
- Sharing experiences, feelings and concerns often helps strengthen personal relationships and resolve difficulties
- Peer support is available through the Kidney Foundation of Canada
Helpful resources
6. In-centre hemodialysis support
- Monitoring is provided by the nursing staff of your Kidney Team
- Certain members of your Kidney Team will visit you weekly on dialysis
- If needed you may request to see a member of your Kidney Team during one of your dialysis treatments






