Limb preservation
Sunnybrook’s Schulich Heart Program is perfecting minimally invasive angioplasty techniques to improve the lives of patients with peripheral arterial disease, a narrowing of blood vessels that can lead to lost limbs and even lost lives.
Using concepts honed in plastic surgery and techniques developed in the cardiac catheterization lab, our vascular surgeons are restoring blood flow to extremities below the knee. Instead of trying to bypass a blocked artery – procedures which typically result in long, painful recovery periods, especially for slow-healing diabetics, Sunnybrook vascular surgeons use angioplasty procedures that clear blockages with a guided coronary wire, then open up the artery more permanently with a balloon. Once blood flow is restored, patients go home the same day without ever having undergone general anesthesia. The goal is to quickly restore our patient’s quality of life.
How it works
Angioplasties are like plumbing. When a pipe gets clogged, our surgeons and cardiologists go in like the plumbing crew of the medical world, and clear the blockage.
- After undergoing ultrasound tests (that detail blood flow and reveal narrowed arteries or blockages), a physical exam and sometimes a CT scan in the clinic, patients head to the catheterization lab for an angioplasty procedure.
- If the patient requires it, some mild sedation may be offered before getting an X-ray of the groin area to determine what will be the safest point of entry to the patient’s femoral artery.
- After administering a local anesthetic, a small surgical cut is made in the groin on the side opposite the problem leg.
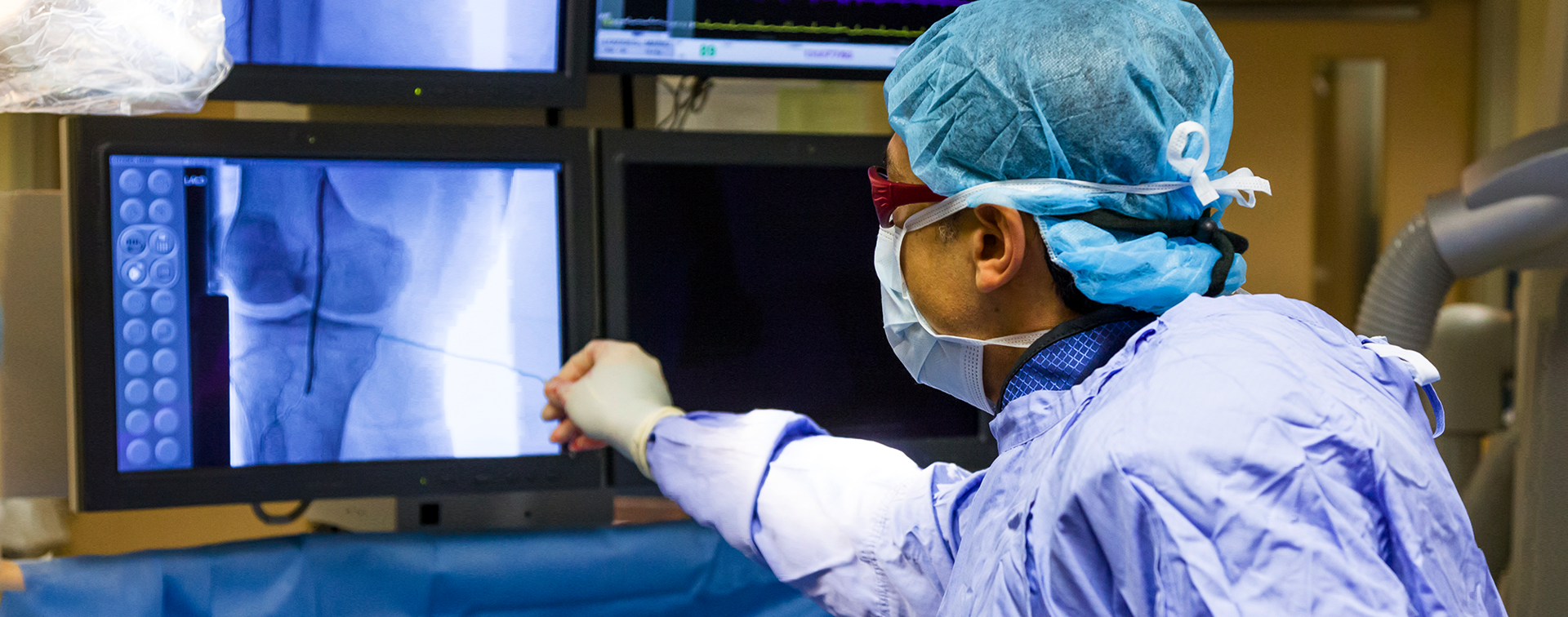
- The artery is then punctured with a needle, and a catheter is fed up and over the middle of the femoral artery, down into the opposite leg. A coronary wire is fed through the catheter. Dye is injected through the catheter, allowing the surgeon to see the blood flow and vessels via moving X-ray pictures (fluoroscopy).
- A blood thinner is administered, then the wire of choice is fed through the catheter down to the target area. The wire is used to clear the blockage, then a tiny balloon is slid down to the site of the angioplasty. Using a small hand pump, the surgeon inflates the balloon inside the artery, leaving it in place for three minutes or so, opening up blood flow through the vessel.
- The balloon, wire and catheter are removed from the patient, and the wound is closed.
- Patients go home four hours after the procedure and return for a diagnostic checkup in a month’s time.
About peripheral arterial disease (PAD)
Peripheral arterial disease (PAD), a complication of diabetes, is an under-recognized but potentially life-threatening condition caused by a narrowing of the arteries. PAD can cause sufferers waves of muscle cramping in the thigh and upper calf, and discomfort in the feet at night or while sitting. Painful sores may develop on the legs or feed and walking for any distance may become impossible. Even with treatment, 40 per cent of people with severe PAD face major amputations. Sunnybrook’s vascular surgeons and scientists are racing to change that devastating outcome.
Incidence of peripheral arterial disease rising
PAD results from a build-up of plaque in the walls of the arteries, blocking the flow of blood to the limbs, most commonly the legs. This vascular disease affects as many as 800,000 Canadians. People with diabetes are two to four times more likely to be affected.
Diagnoses often come too late to save a limb that has developed gangrene and amputation is the only option. An estimated 2,000 people with diabetes in Ontario loses a limb each year. With rates of diabetes steadily rising, a number of patients suffering amputations is projected to increase by 50 per cent over the next 20 years. Our vascular surgeons and scientists are taking the lead in ensuring that won’t happen, working to raise awareness of the disease and to invent and offer the most advanced treatments to eliminate amputations.
Leading the way to advancing treatments
Until recently, bypass surgery was the standard treatment for PAD. Sunnybrook’s vascular surgeons, however, have achieved widespread recognition for using minimally invasive angioplasty to clear blockages and restore blood flow to patients’ legs. The procedure involves sending a balloon in a catheter through tiny arteries in the leg to open the blood vessels leading to the foot. Patients who could barely walk often experience immediate relief and typically return home the same day. Our surgeons perform 250 of these procedures annually.
Sunnybrook is one of the first Canadian centres to offer a new option to reduce the need for repeat procedures. We use a drug-coated balloon angioplasty that delivers a drug directly in the wall of the artery. The drug minimizes scar tissue formation, which can lead to blockage of the artery.
How we’re making a difference
 Abram’s Story: Preserving limbs, saving lives
Abram’s Story: Preserving limbs, saving lives
"I’m so thankful that my feet have improved so much. I am walking well, and I can even dance a bit again so I am happy."
 Christopher’s Story: Innovative procedure saves limbs and lives
Christopher’s Story: Innovative procedure saves limbs and lives
Vascular surgeons at Sunnybrook are pioneering a procedure typically used for heart patients to save the legs of diabetics with foot ulcers.
Refer a patient
Send us an eReferral or search for us on the Ocean Healthmap.