In-hospital care after your surgery
How will I feel after my surgery?
After the surgery is done, you will wake up in the Cardiovascular Intensive Care Unit (CVICU). When you wake up, you may notice a lot of tubes and equipment. Please do not be concerned; a nurse will be tending to you and the equipment.
After your surgery, you may feel...
- You may have a sore throat and hoarseness from the breathing tube that was in place during your surgery.
- You may feel tired from the medications you were given.
- You may have some bruising and tenderness in the area of your operation.
- You will continue to get pain medication through your intravenous catheter (IV) in your arm. The IV stays in for approximately 2 to 3 days.
- Medications may cause temporary delirium. You may have restraints on your arms if you are at risk of harming your care.
Most patients admit they do not remember the first few days after surgery.
Inpatient progress tracker
Your health-care team will help you get moving throughout your stay in the CVICU and inpatient unit. You can our printable checklist to track your progress. The progress tracker follows our expected pathway to recovery, but recovery is different for each person. Please do not be discouraged if your progress isn’t exactly as shown.
Download the inpatient progress tracker
Getting moving
Getting moving after surgery can help prevent some common complications such as pneumonia, blood clots in the legs, and muscle weakness or stiffness. Your nurse will help you sit over the edge of the bed and dangle your feet within the first 8 hours after your surgery. They will also help you sit in a chair for all your meals.
On the first day after surgery, a physiotherapist will assess you and assist you with deep breathing, coughing, exercises and general mobility.
Don't fall, call:
Please call for assistance when you need help getting up. Wear non-slip footwear and any aids such as glasses, hearing aids and a walker to help prevent you from falling.
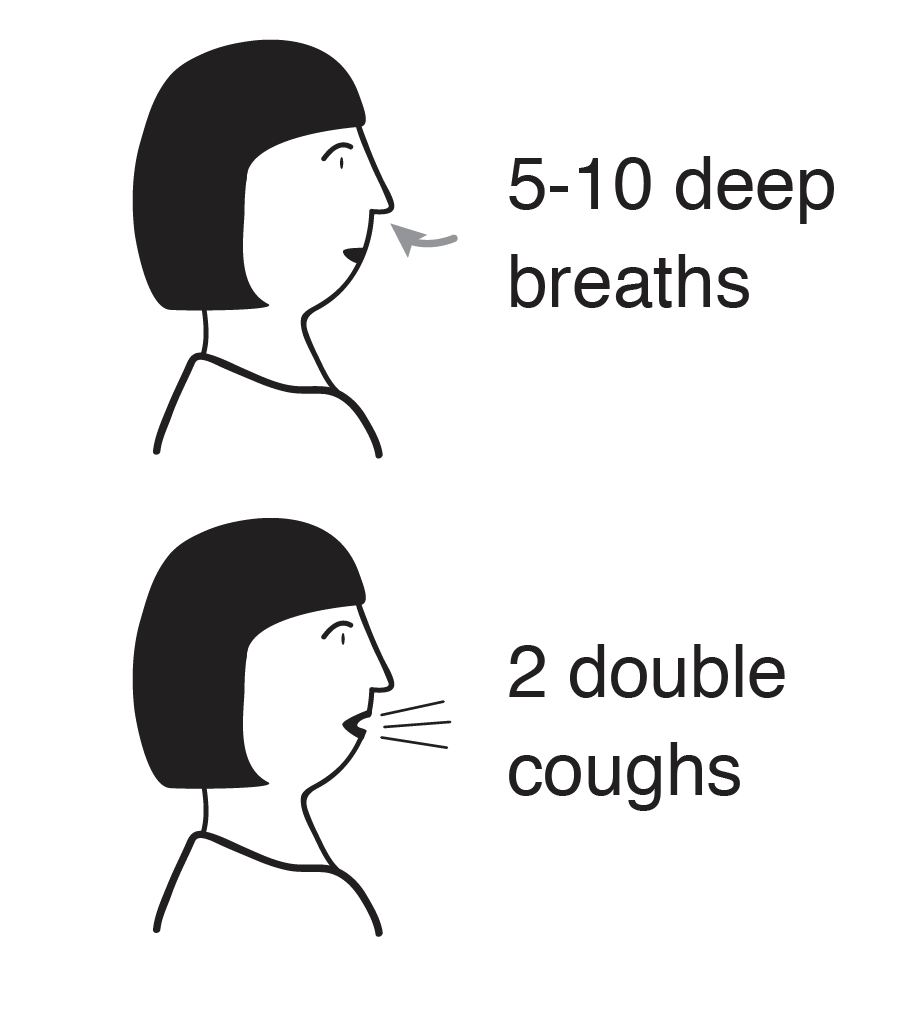
Deep breathing and coughing
Breathing deeply gets air down to the bottom of the lungs. It helps clear mucus to prevent you from getting a lung infection. Breathe in deeply through your nose until your lungs feel full of air. Hold the air in your lungs for 2 to 3 seconds, and then slowly breathe out through your mouth. Repeat 10 times.
After your breathing exercises, hug your chest and have tissues ready. Take a deep breath in followed by a strong cough. Repeat this two times. Coughing may be uncomfortable, but it will not cause any damage to the breastbone.
Practice deep breathing and coughing every hour you are awake.
| Repititions | Frequency |
|---|---|
| 1 | Hourly |
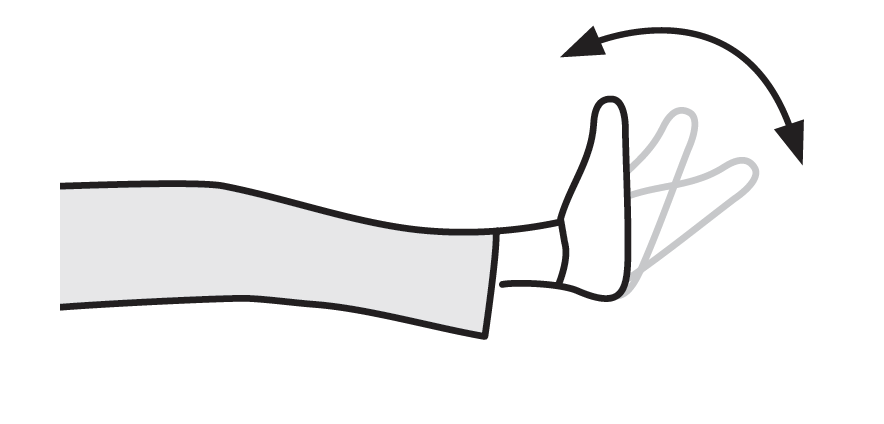
Ankle pumps
Pumping your ankles can help circulation. Pull your toes toward you and then push down like on a gas pedal. Repeat 10 times. Practice ankle pumps every hour you are awake.
| Repititions | Frequency |
|---|---|
| 10 | Hourly |
Walking
Walking usually begins on the first day after surgery when you are on the inpatient unit. You will need some help at the beginning.
You may be using a walker and/or portable oxygen. By the third day, most people are able to walk short distances on the unit with little assistance. Walks last 3 to 4 minutes at a comfortable and safe pace, three times a day.
| Repititions | Frequency |
|---|---|
| 3 | Daily |
Swelling
It is common for your legs to swell after heart surgery. Here are ways you can help decrease swelling and improve circulation:
- Do ankle pumping, lower leg exercises, and walk frequently. Avoid standing or sitting for long periods of time.
- When resting in bed, use pillows to raise your legs higher than your heart. When sitting in a chair, elevate your feet using a foot stool.
- You may be instructed to wear compression stockings.
- DO NOT cross your legs – this limits blood flow.
Swelling should decrease within a few months. If you notice persistent swelling in both ankles, let your doctor know.
While in hospital
In the days after your surgery, it is normal to experience some discomfort. This is temporary. During your inpatient stay at Sunnybrook, your health-care team will work with you to get you the care you need.
Nutrition
Good nutrition is important for your recovery after surgery. Avoid any weight loss until you have recovered from your surgery and your incisions have healed.
After surgery, you will start with clear fluids like broth, juice or Jell-O. Over the next couple of meals, you will progress to full fluids like porridge, milk or pudding, and finally to heart-healthy meals that are low in fat, cholesterol and salt. Many patients experience poor appetite, nausea, and change in taste after surgery. This usually resolves in time.
Ask the nurse if you want to speak to a dietitian during your stay. A dietitian can work with you to improve your nutrition by discussing your food preferences, adjusting your diet in hospital and offering nutritional supplements if necessary.
Emotional changes
It is common to become sad, depressed or more emotional after any major surgery. It is often related to the anesthesia, medications, lack or loss of sleep, and stress. Your loved ones may also experience several emotions, including helplessness, fear and overprotectiveness. These feelings may come and go over a period of time and usually pass in 6 to 12 weeks. If these feelings continue for several months after your surgery, please speak with your family doctor.
Delirium
After surgery, you may experience temporary changes to your thinking and behaviour. You may become disoriented, forgetful or have difficulty thinking clearly. Your health-care team will ask you questions to assess for signs of delirium and determine the best ways to help prevent or manage your condition.
Pain and discomfort
Each patient experiences pain and discomfort in a different way. After heart surgery, you may feel discomfort in the chest and wound sites for several weeks as you heal. This pain may also be in your arms, neck and shoulders. The pain has been described by patients as a dull ache, stiffness or pulling sensation and is usually relieved by pain medication.
If the medication is not providing relief, or you are having angina or other chest pain, speak with a member of your health-care team.
Constipation
Constipation is common as a result of your pain medication, reduced activity levels or iron supplements. While in hospital, you may be given a laxative to avoid straining your body. If constipation continues to be a problem, talk to a pharmacist or your doctor.
Medication
Changes will be made to your medications after your surgery. New medications may be added for long-term heart protection, and you may be prescribed some temporary medications to help with pain or constipation after surgery. Some of your previous medication such as blood pressure medications, diabetes medications, or blood thinners may be adjusted or discontinued.
A new prescription will be given to you on the day that you are discharged – this prescription will be a complete list of all the medications you are to take when you go home. A member of your health-care team will review your medications with you before you go home. Your family doctor, cardiologist, or surgeon will review these medications on your follow-up appointments and provide refills as needed.
Fill your discharge prescription on the day you go home to avoid missing any medications. You may fill your prescription at Sunnybrook’s ambulatory patient pharmacy on the first floor of M-Wing or at your local community pharmacy.
If you have any questions about your medications and potential side effects, contact your doctor, nurse practitioner or pharmacist.
Sleeping
It is important to your recovery to rest and sleep. After surgery, it is common to have temporary changes of sleep habits. You may have difficulty sleeping because of pain or anxiety. Consult your doctor if you have trouble sleeping.
Infection control
Please clean your hands each time you enter and leave your room and unit using the hand sanitizer stations throughout the hospital. Friends and family should not visit you if they are sick.

Preparing to go home
Your health-care team has evaluated your progress since your operation and has decided that you are ready to leave the hospital. By the time you are discharged you should be able to take frequent walks around the inpatient unit on your own and have a shower.
The recovery period after you leave is individual and can last for 6 to 12 weeks. How long you spend recovering depends on your age, activity level before surgery, general health and your progress in hospital. Do everything in moderation.
We recommend someone be available at home to assist you. You will feel tired, and normal tasks such as showering or preparing food might be more challenging than usual. To let your breastbone heal, you will not be allowed to lift anything greater than 2.3 kilograms (5 pounds) – which is almost everything.
Your discharge checklist
- Arrange to be picked up by 11 a.m. on the day of discharge. Make sure your family brings you loose fitting clothing on the day before you go home.
- Speak to your physiotherapist about follow-up exercises and outpatient cardiac rehabilitation programs. A discharge class is scheduled every Monday, Wednesday and Friday at 10:30 a.m. in the patient lounge on D3.
- Review the discharge paperwork with your nurse, including follow-up appointments and letters for your family doctor.
- Review your discharge prescriptions with your doctor, nurse or pharmacist.
- Arrange for someone to be home with you or nearby for the first week to help you, if you haven’t done so already. Remember you will not be able to lift more than 2.3 kilograms (5 pounds).
- Bring this booklet home with you. It contains information about your home recovery program.






