What is spontaneous coronary artery dissection (SCAD)?
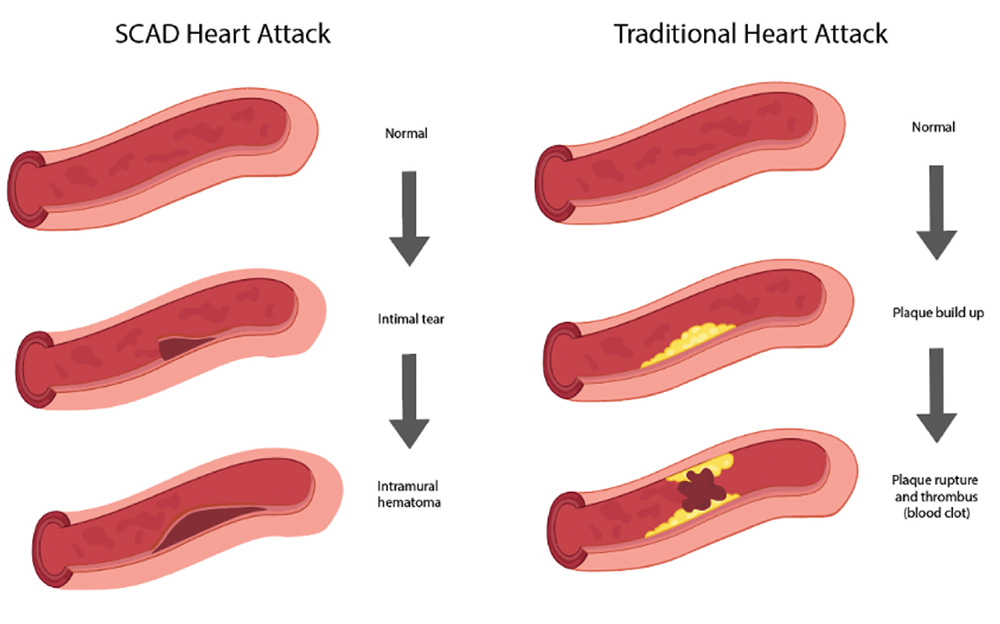
Spontaneous coronary artery dissection (SCAD), is when there is a sudden tear in the wall of one or more blood vessels in the heart. This results in a buildup of blood between the layers of the artery wall. As blood collects between the layers of the wall, the vessel narrows. This impairs blood flow to the heart which causes a heart attack.
Figure 1: SCAD heart attack versus traditional heart attack.
How common is SCAD?
SCAD makes up 4% of heart attacks across the world. In women less than or 50 years of age, SCAD is the cause of 35% of heart attacks. SCAD is the number one cause of heart attacks in pregnancy.
 Who gets SCAD?
Who gets SCAD?
SCAD is most common in middle-aged women between the ages of 45 to 55. Less than 10-15% of SCAD cases occur in males.
What are potential causes and risk factors for SCAD?
It is unclear what causes SCAD. In more than 20% of cases there is no known cause. We do know that:
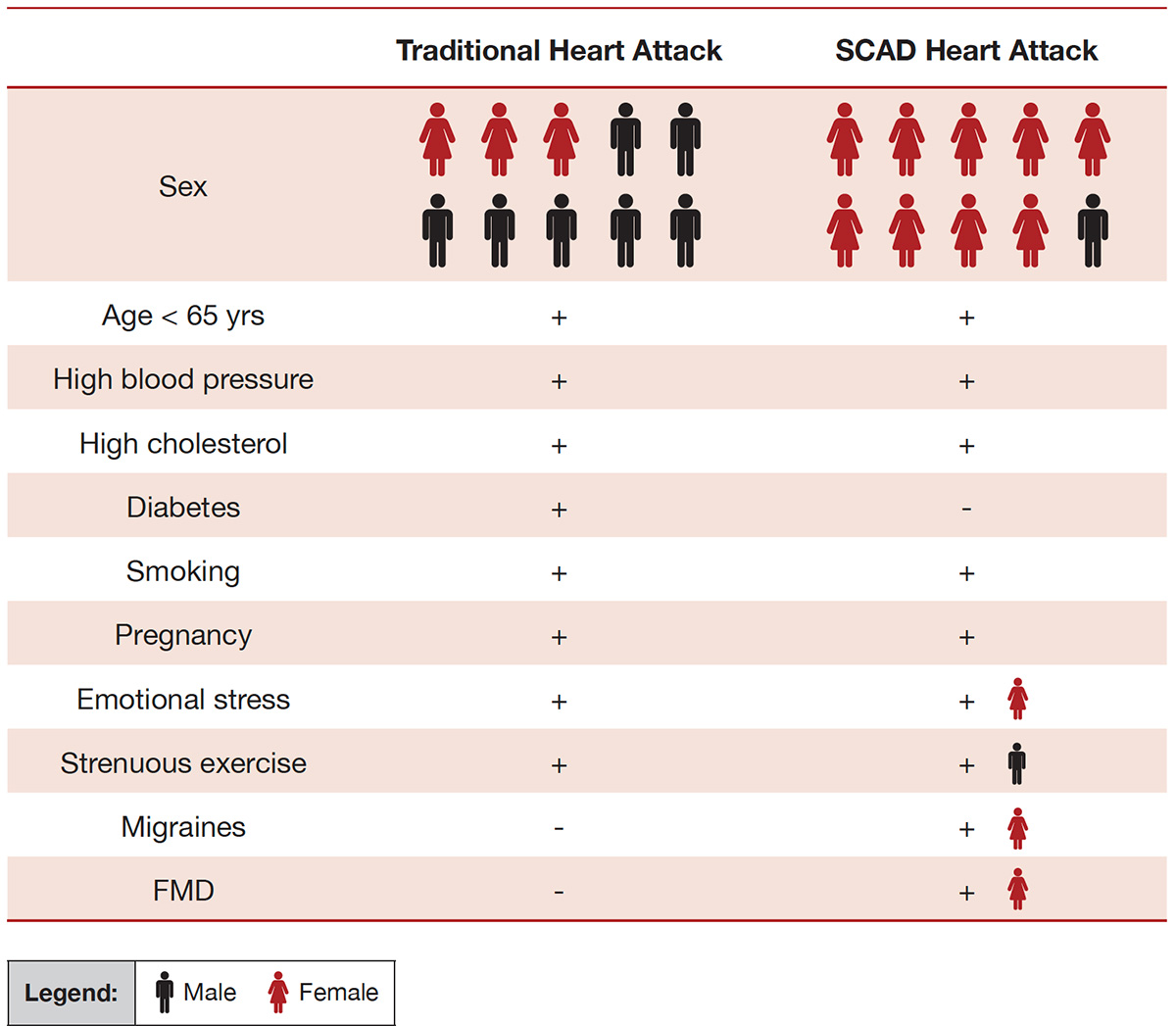
- Sex: SCAD affects many more females than males.
- Fibromuscular dysplasia (FMD): This is a condition with abnormal twisted blood vessels throughout the body with areas of vessel narrowing and dilation. It most commonly affects blood vessels in the heart, the head and neck, and the kidneys. This condition has been found in more than 60% of SCAD patients.
- Pregnancy: SCAD can occur during and right after pregnancy. It has been shown to be more common in females who have had more than one pregnancy or births.
- Emotional and physical stress: Patients with SCAD have higher rates of physical and emotional stressors (for example: loss of a loved one, a job or a relationship, work stress.).
- Connective tissue disorders: This is a group of disorders involving tissue that connects structures of the body together. About 3 to 4% of SCAD is linked to underlying connective tissue disorders. These include Marfan’s syndrome, Ehlers-Danlos and Loey-Dietz syndrome.
- Hormonal therapy: Although up to 10% of patients with SCAD were taking hormonal therapy, so far there is no conclusive evidence that hormonal therapy causes SCAD or increases the risk of SCAD recurrence.
- Genetics: SCAD is rarely associated with a family history. Very few genes have been identified that have an association with SCAD. Some of these gene mutations are familial including F11R and TLN1. Other gene mutations are spontaneous including TSR1, PHACTR1 and EDN1. Further research is needed to help understand whether there is a genetic basis for SCAD.
How are SCAD heart attacks different from regular heart attacks?
Compared to regular coronary artery disease, SCAD patients have lower rates of traditional cardiovascular risk factors. SCAD patients have lower rates of high blood pressure, high cholesterol, diabetes, and smoking. Patients with SCAD report higher rates of emotional and physical stressors.
Table 2: Key differences in demographics and associated conditions in SCAD compared with traditional coronary artery disease (CAD) (adapted from Adlam, García-Guimaraes, et al., 2019).
Signs and symptoms
The majority of patients with SCAD have new chest pain, much like a regular heart attack.
Other symptoms may include:
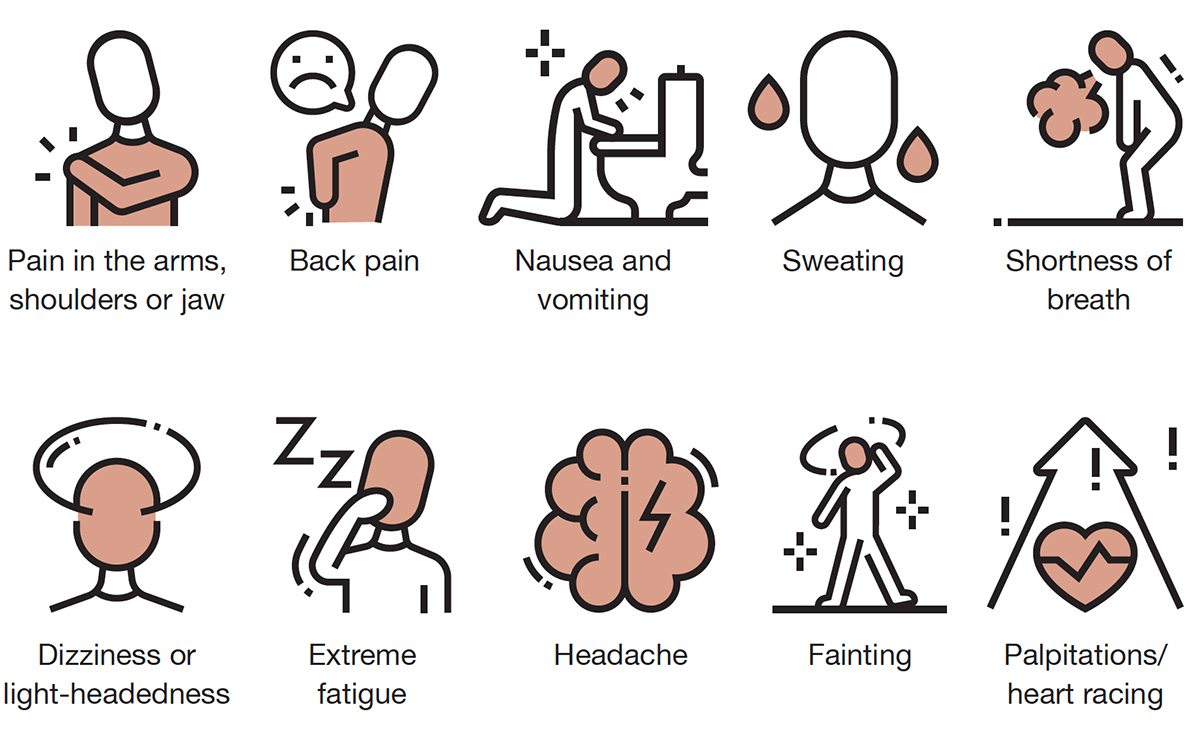
Rarely, patients can have more severe symptoms including dangerous heart rhythms known as ventricular tachycardia and ventricular fibrillation (2-8%), cardiogenic shock (a life-threatening condition where your heart can’t pump enough blood to your organs) or sudden death.
Diagnosis
The first tests used to diagnose SCAD are the same as those used to diagnose traditional types of heart attacks. Patients usually have abnormal electrocardiograms (ECGs) and elevated heart blood markers, known as troponins. The best test used to diagnose SCAD is a coronary angiogram.
A coronary angiogram is an imaging test during which contrast (x-ray dye) is injected into the arteries of the heart (coronary arteries) and x-ray images are used to look for artery narrowing. Classic findings on a coronary angiogram can help differentiate SCAD heart attacks from traditional heart attacks.
In some cases, more imaging from within the coronary arteries is needed to help make a diagnosis of a SCAD heart attack versus a traditional heart attack. These include optical coherence tomography and intravascular ultrasound. These are performed at the same time as the coronary angiogram, if needed.
Other non-invasive imaging studies such as computed tomography angiography or magnetic resonance angiography are less useful to make the initial diagnosis of SCAD, but help to screen other large blood vessels for abnormalities like FMD or aneurysms.






