Scientists uncover which gene could help boost immune systems
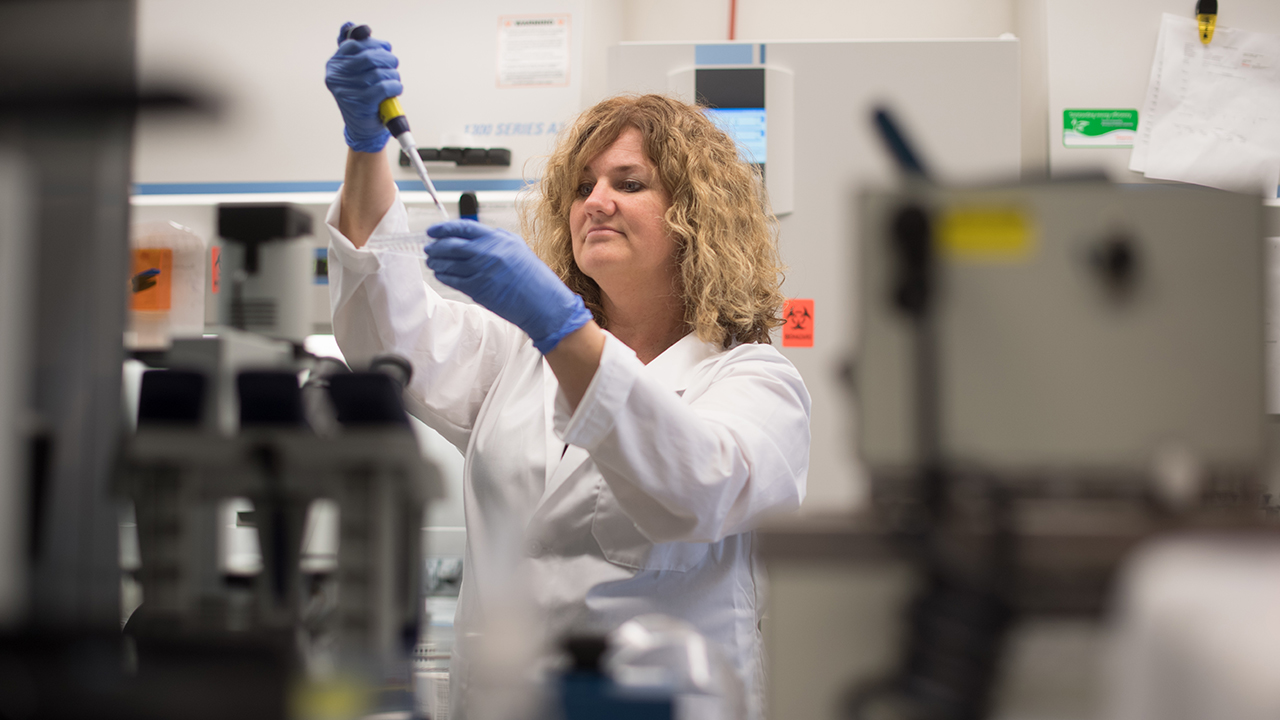
In the pursuit of making immune-boosting T-cells for people who need them, Sunnybrook scientists used gene-editing technology known as CRISPR-Cas9 to single out which gene in our bodies is doing a big chunk of the work in their development.
CRISPR-Cas9 is the same technology scientists are using to change the colours of flowers, and potentially restore sight to inherited blindness. But scientists at Sunnybrook Research Institute have used it to unearth a gene workhorse in T-cell development – a fundamental part of our immune system – known as HEB.
HEB is a transcription factor gene that can turn on or off various genes throughout cell development like a light switch. According to the study published in Stem Cell Reports, its ultimate power, though, is turning on T-cell genes and turning off others that could impact their growth.
“T-cells are vital to our immune system: without them we’d get sick and could die very quickly if we contract a virus or bacteria that threatens our health,” says Michele Anderson, senior scientist at Sunnybrook Research Institute and associate professor in the Department of Immunology at University of Toronto. “While T-cells can already be engineered from stem cells, they cannot yet be produced at the quantity and purity needed to make them beneficial for clinical use.
By being able to engineer more, pure T-cells, we’d be able to put them into people who need them – people with AIDS, those who are undergoing radiation therapy or bone marrow transplants, anyone really with an immunodeficiency.”
Until now, the significance of HEB has only been known in mice; its importance in human biology remained uncertain. It was this gap in knowledge that prompted Anderson, fellow senior scientist Juan Carlos Zúñiga-Pflücker, also a professor and Chair of the Department of Immunology at University of Toronto, and their colleagues at Sunnybrook, to investigate.
Using CRISPR-Cas9, which are like molecular scissors that can cut, edit or correct DNA, scientists snipped out HEB from human pluripotent stem cells (master cells that have the ability to form any cell type) and watched how the cells developed.
The study says the lack of HEB partially blocked the ability for the stem cell to form a tissue type known as mesoderm, and the ability to make tissues that arise from mesoderm such as blood and heart muscle cells. Any cells that made it through the block were blocked again at a later stage in cell development when they were meant to develop into what’s known as hematopoietic cells, which give rise to T-cells and all other blood cells.
“Without HEB the surviving stem cells no longer had the capacity to become T-cells,” says Anderson, one of the study’s lead authors. “When we put HEB back into the equation, the deficiencies disappeared.”
Anderson and her colleagues are now looking at how they can harness the power of HEB to engineer enough pure T-cells to finally benefit humans. But she notes that future steps also include analyzing other human diseases that involve mesodermal tissues and may be connected to the HEB gene as well, particularly in the heart.
This study was funded by Canadian Institutes for Health Research, National Institutes of Health, and the Krembil Foundation.
For media interviews, please contact:
Katherine Nazimek
Sunnybrook Health Sciences Centre
katherine.nazimek@sunnybrook.ca
416-480-4040