Full media release
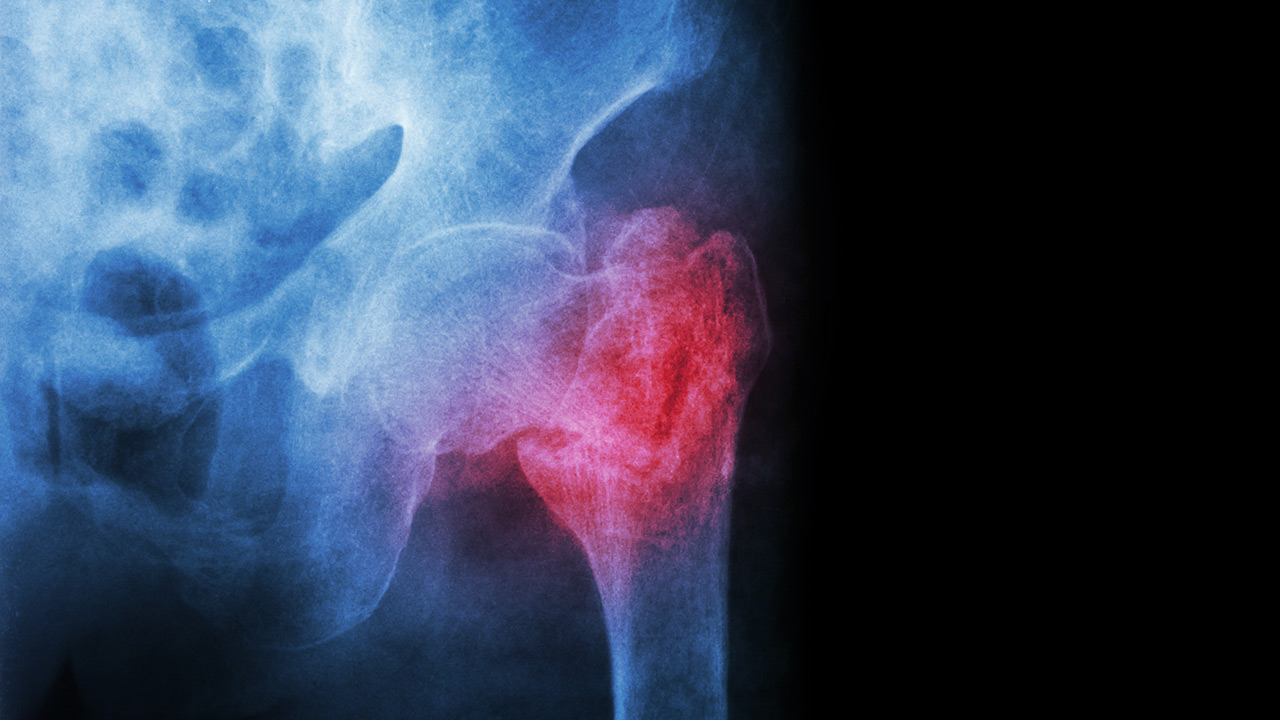
HIP FRACTURE SURGERY AFTER MORE THAN 24 HOURS ASSOCIATED WITH INCREASED MORTALITY RATES AND OTHER COMPLICATIONS
Hip fracture surgery at 24 hours from hospital arrival may signal a significant threshold, defining higher risk for mortality and other complications, reports a new study from researchers at Sunnybrook Health Sciences Centre and the Institute for Clinical Evaluative Sciences (ICES).
The study published in The Journal of the American Medical Association (JAMA), is the first to measure and determine a specific time-to-surgery point at 24 hours, after which the risk of mortality and developing complications begins to increase. Complications analyzed included heart attack, pneumonia, deep vein thrombosis and pulmonary embolism.
Hip fracture surgery is already the most commonly performed urgent procedure in Canada, and numbers are increasing exponentially due to the aging population. Current guidelines in Canada and the United States recommend surgery within 48 hours, whereas 36 hours is the standard in the United Kingdom.
“Despite extensive research already conducted on the topic, an optimal time for surgical treatment remains a point of contention. In identifying a specific risk threshold, our hope is that this will help inform guidelines worldwide and improve unnecessary delays in treatment for patients with these devastating injuries,” says Dr. Daniel Pincus, study author, orthopaedic resident physician at Sunnybrook, PhD student at the University of Toronto who works with ICES data and researchers.
Patients receiving hip fracture surgery after 24 hours had significantly higher risk of increased mortality rates and other complications, within 30 days, compared to patients who had surgery earlier (12.2 per cent or 1,680 patients versus 10.1 per cent or 1,383 patients). Only 33 per cent of patients in the study received surgery within 24 hours.
“These findings apply to other countries where operating room resources are limited and patients are required to wait for hip fracture surgery,“ says Dr. Pincus. “Since wait times for hip fracture surgery are already used worldwide as quality indicators to assess hospital performance, the results may directly inform current practice and patient care.”
Researchers examined data from a population-based cohort of 42,230 patients who had hip fracture surgery in Ontario between April 2009 and March 2014. The median age was 80 years, and over 70 per cent of these patients were women.
“Treatment within 24 hours has now been shown to be associated with fewer complications. However, we recognize that early hip fracture treatment must be balanced with the needs for other surgical procedures and know there are practical and resource challenges. Future work should try to identify a subset of patients in most need of urgent surgery. Also whether early surgery reduces the costs of medical care,” adds Dr. Pincus.
Authors: Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens A, Kreder H, Jenkinson R, Wodchis W.
This study was generously supported by the Marvin Tile Chair in Orthopaedic Surgery at Sunnybrook Health Sciences Centre, and by the Institute for Clinical Evaluative Sciences.
Sunnybrook Health Sciences Centre is inventing the future of health care for the 1.2 million patients the hospital cares for each year through the dedication of its more than 10,000 staff and volunteers. An internationally recognized leader in research and education and a full affiliation with the University of Toronto distinguishes Sunnybrook as one of Canada’s premier academic health sciences centres. Sunnybrook specializes in caring for high-risk pregnancies, critically-ill newborns and adults, offering specialized rehabilitation and treating and preventing cancer, cardiovascular disease, neurological and psychiatric disorders, orthopaedic and arthritic conditions and traumatic injuries. The Hospital also has a unique and national leading program for the care of Canada’s war veterans. For more information about how Sunnybrook is inventing the future of health care please visit us online at www.sunnybrook.ca
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
FOR FURTHER INFORMATION PLEASE CONTACT:
Natalie Chung-Sayers
Communications Advisor, Sunnybrook
natalie.chung-sayers@sunnybrook.ca
(c) 416-710-3740 (o) 416-226-6780 ext. 7297
Deborah Creatura
Media Advisor, ICES
deborah.creatura@ices.on.ca
(o) 416-480-4780 or (c) 647-406-5996