Inflammation to blame for Alzheimer’s, blood-test marker identified
A new study provides concrete evidence that an inflammatory response from the immune and nervous systems may contribute to the development of Alzheimer’s disease in the brain.
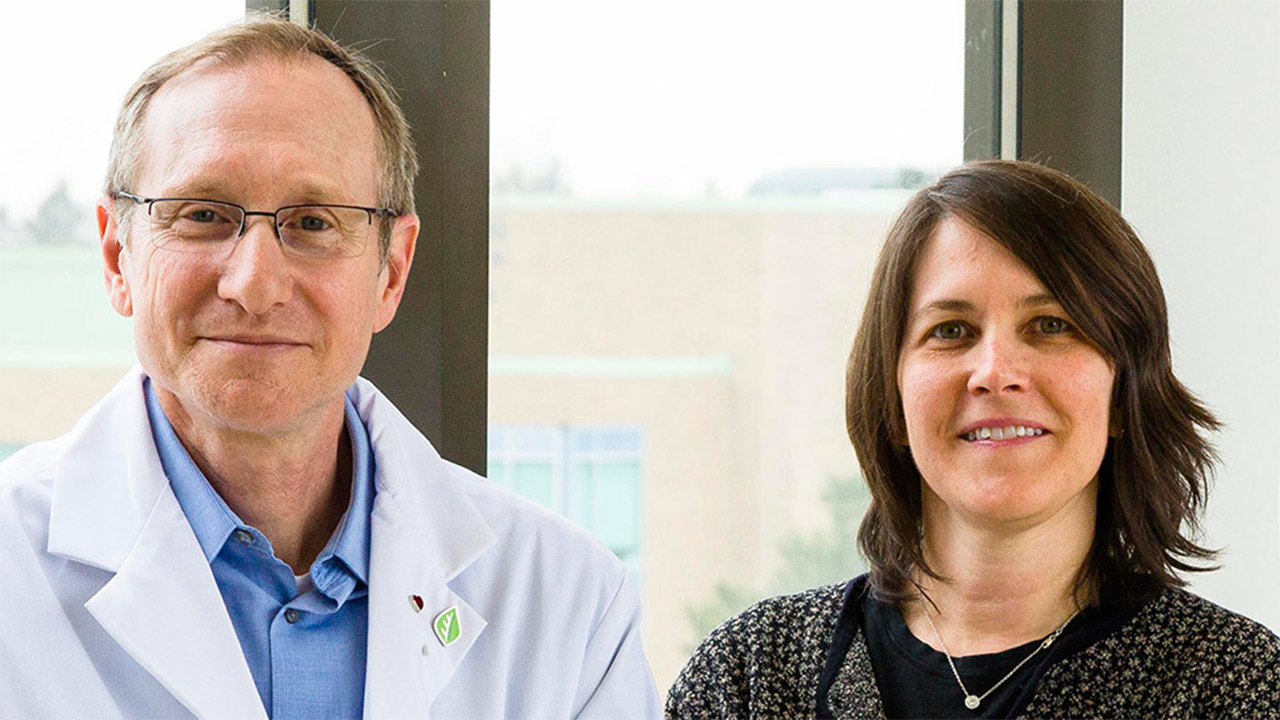
"Increasing evidence suggests that elevated levels of inflammation in the brain and blood are involved in Alzheimer’s disease (AD) pathology, and our findings have not only validated this, but have also identified a blood test marker (IL-6) that correlates with the severity of the illness, which means it can potentially be used to stage the illness (determine whether it is mild, moderate or severe) and monitor treatment response,” says Dr. Nathan Herrmann, senior author of the study and the Richard Lewar Chair in Geriatric Psychiatry at Sunnybrook and University of Toronto. “Now we have to determine if and how this information may be useful in the care of patients.”
Published in the August 2017 issue of the Journal of Neurology, Neurosurgery and Psychiatry, the researchers conducted a meta-analysis of 175 studies involving over 13,000 patients with AD and over 12,000 healthy patients. The paper summarized the original reports containing measurements of over a dozen inflammation levels in the blood of AD patients compared to healthy individuals.
“Six pro-inflammatory molecules (or blood markers) were found to be significantly elevated in patients with AD compared with healthy controls, indicating chronic inflammation in AD,” says Celina Liu, a PhD student in the Neuropsychopharmacology lab at Sunnybrook under the supervision of Dr. Krista Lanctôt. Enzyme levels were also elevated in AD patients compared to healthy controls.
IL-6 was shown to be extensively investigated in studies as a pro-inflammatory protein found in the blood that plays a critical role in the inflammatory cascade and can accelerate ongoing neurodegenerative processes in AD.
“We suspect that inflammation plays a crucial role in the early stages of disease when intervention may be most beneficial,” adds Dr. Herrmann, also the head of the Division of Geriatric Psychiatry at Sunnybrook and a professor of Psychiatry at University of Toronto. “Our hope is that the detection of biomarkers of AD may allow for the development of novel therapeutics for the prevention and treatment of AD.”