White Matter Affects Alzheimer's Treatment
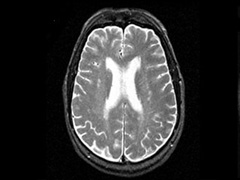
Researchers at Sunnybrook have shown that there may be a difference in response to treatment in Alzheimer’s Disease (AD) patients with and without white matter disease in selective areas of the brain.
White matter disease (WMD) is a common condition of the brain that can impair one’s cognitive abilities, in particular with aging. About 40 per cent of the brain is made up of white matter, which is the area where everything connects. The disease involves lesions in the white matter of the brain that can occur when blood supply is disrupted as a result of hardening of tiny arteries, which then damages the connecting pathways and can affect brain function, one of which may include the ability to plan and problem-solve.
A new scale was developed by Dr. Sandra Black’s team at Sunnybrook Health Sciences Centre to measure the amount of WMD in areas of the brain that play a key role in attention, learning and memory. Further research in Dr. Black’s lab by her PhD student Pearl Behl and colleagues showed that treated AD patients with more strategically placed white matter disease in selective pathways showed less decline in executive functioning and working memory. These functions are primarily controlled by the left frontal lobes of the brain. This area allows one to hold information and manipulate it for use in problem solving, and reasoning while doing something else, for example.
“We asked ourselves: whether having WMD selectively located in strategic areas of the brains of AD patients would affect response to treatment in these patients?” says Pearl Behl, a Sunnybrook scientist. “We were interested in investigating whether location of the WMD would matter and wanted to learn whether having the disease in specific areas of the brain versus total white matter disease in the whole brain would have an impact on response to treatment in these patients.”
White matter is that part of the nervous system which is composed mainly of the fibres or axons of nerve cells, most of which are covered by whitish, fatty sheaths. “96 per cent of the population gets white matter disease with age,” says Pearl, now a medical student at the University of Toronto. “Studies are lending credibility to the idea that white matter lesions, caused in part by vascular risk factors such as hypertension, diabetes and high cholesterol, play a role in the evolution of AD dementia.”
“Patients with AD treated with cholinergic drugs who had a high level of WMD in the cholinergic pathways showed less decline over one year on executive and working memory tasks, whereas no differences emerged in overall white matter disease burden,” says Pearl.
In this research, neuropsychological assessments were conducted using memory and language tests, visuospatial function tests, working memory and executive functioning tests, and activities of daily living. The study showed that Alzheimer patients with a higher amount of WMD in selective areas of the brain’s white matter declined less with cholinergic treatment on some frontal tasks than those with less WMD in these pathways.
“Our data suggest that white matter changes previously described as ‘non-specific’, when in strategic locations within the brain, may modulate responsivity to treatment in AD,” says Pearl. “However, this study looked at strategic involvement of selective pathways involved in AD and therefore may explain only part of the story. There are other pathways that overlap and intermingle in the same areas as the fibres we looked at, that are also important for working memory and executive control. This is only one part of the puzzle and there is still a lot of work that needs to be done.”
PDF / View full media release »