Hijacking of blood vessels may promote cancer resistance
Sunnybrook researchers show for the first time, that a cancer initially responsive to anti-angiogenic therapy may become resistant by hijacking an organ’s existing blood vessels, as reported in a preclinical study published in the Journal of the National Cancer Institute.
Anti-angiogenic drugs inhibit “tumour angiogenesis” or the formation of new blood vessels from pre-existing ones, which tumours need for their progressive growth. Over time, cancers can become resistant to these drugs. It has been speculated that one way this may happen is by hijacking the existing blood vessels in organs such as the liver – a process called “vessel co-option”. This is now reported by the Sunnybrook researchers.
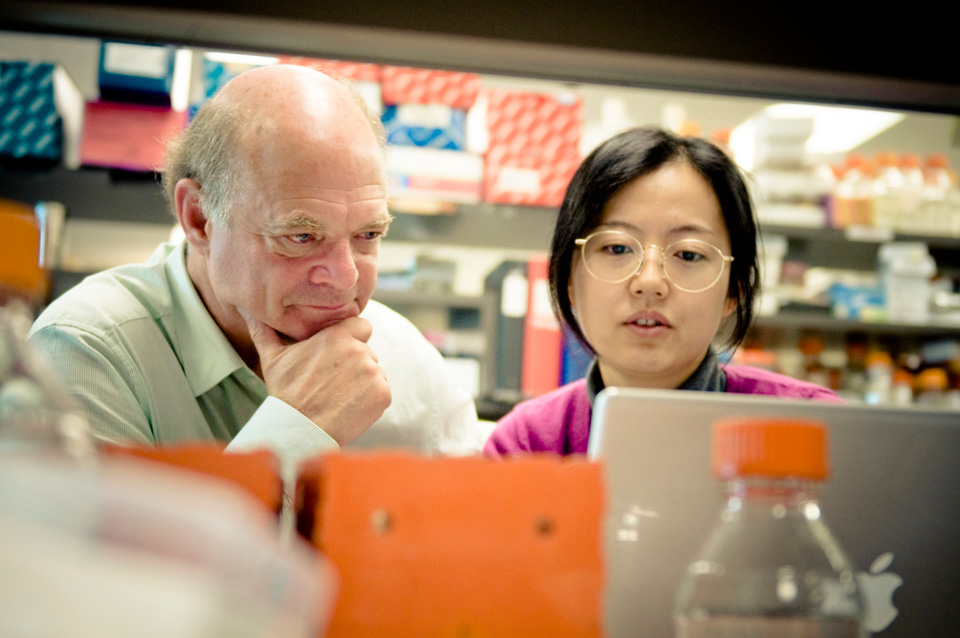
“It is our hope is that our findings will propel more research into resistance mechanisms and ways to target them,” says Dr. Robert Kerbel, lead investigator, senior scientist, Sunnybrook Research Institute and professor, Medical Biophysics, University of Toronto.
The study led by Sunnybrook Research Institute in collaboration with Dr. Andrew Reynolds at The Institute of Cancer Research in the UK looked at how resistance happens in advanced liver cancer (late stage hepatocellular carcinoma) upon treatment with sorafenib, an anti-angiogenic drug.
The researchers suggest that during acquired resistance, the cancer cells switch from relying on angiogenesis, to vessel co-option. “This research adds to the growing idea that angiogenesis is not always necessarily essential for cancer growth. It could also help explain why conventional anti-angiogenic drugs often have a limited benefit,” says first author, Dr. Elizabeth Kuczynski, post-doctoral fellow, Sunnybrook Research Institute.
Findings include:
- Liver cancer cells became more invasive over time, resulting in the incorporation of liver tissue and its vessels into the tumour. The researchers suggest that cancer cells developed EMT-like (epithelial-to-mesenchymal transition) molecular changes that facilitated invasion.
- Angiogenesis was blocked throughout treatment and contrary to expectations it did not return during resistance. Regions of tumour perfusion or blood delivery during resistance corresponded to vessel co-option. The researchers used a unique high-frequency contrast ultrasound imaging technique with microbubbles developed by study collaborator, Dr. Stuart Foster, Sunnybrook Research Institute, that allowed for highly accurate, localized, microvascular assessment of tumour perfusion.
- Elastic effect - if the anti-angiogenic drug treatment was stopped during acquired resistance, the tumors resumed angiogenesis activity. The researchers suggest that this reversible effect may explain why cancer can once again be responsive to the same anti-angiogenic drug after a period of resistance.
“Currently, there are no agents that can discern co-opted vessels from angiogenesis ones to target them for therapy, but there are potential agents that can target the pre-invasion process. Further research in this direction may be the potential key to a better understanding of how to modulate therapies in order to mitigate resistance in advanced cancers,” says Dr. Kerbel, who collaborates with medical oncologists at the Odette Cancer Centre, Sunnybrook Health Sciences Centre, and other healthcare institutions.
This study was generously funded by the Canadian Institutes for Health Research (CIHR), the Canadian Liver Foundation, Worldwide Cancer Research, and Breast Cancer Now.
Read more about this study at Sunnybrook Research Institute (SRI) »