Patient Education: Diseases Conditions Treatments & Procedures
Osteoporosis (Spine)
Overview
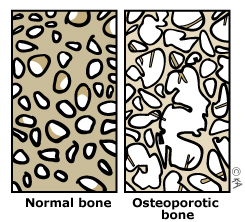
Primary osteoporosis occurs in individuals when there is no other disease or disorder to account for changes in bone mass. We define osteoporosis when one's bone mass is 67% below age-adjusted average bone mineral density. Peak bone mass occurs in the third decade of life and thereafter bone loss occurs at a rate of 0.3% per year in men and 0.46% per year in women. This increases to 2% to 3% at menopause. It is recommended that you discuss with your primary care physician whether a bone density scan is indicated for you. A complete history including family history and drug history will help make this determination. If indicated your doctor should start you on the appropriate medical management for protecting your bone stock and minimizing your bone loss. Don't forget to exercise, as this is one of the best ways to slow down osteoporosis.