Vaginal dryness
Vaginal dryness as a result of menopause can significantly alter a young woman’s quality of life. This pamphlet will explain the causes and symptoms of vaginal dryness, and suggest techniques to manage it and counteract its ill effects.
It’s important to understand what is happening to your vagina while you are in a menopausal state. With decreased female hormones such as estrogen, the healthy, moist lining of the vagina begins to thin out and becomes dry and prone to tearing. This is referred to as vaginal atrophy. It may not be noticeable at first, but when you experience hot flashes and other menopausal symptoms, the process of vaginal atrophy has already begun.
As vaginal atrophy progresses, the vagina becomes dryer and shorter and the opening starts to narrow. As the vagina loses its moisture and elasticity, sexual intercourse becomes more and more painful and may lead to vaginal bleeding. The vaginal pH also changes, making the vagina less acidic and more prone to yeast and other infections.
Vaginal dryness is best dealt with by being proactive to prevent the structural changes described above. You’ll need your own “Tool Box” containing: vaginal moisturizers, lubricants and a set of dilators of various sizes. In addition, exercises targeted to strengthen and maintain pelvic strength will help keep the vagina healthy and strong.
It is helpful to know the order in which to use vaginal care products. Always start by moisturizing, then add lubricants and dilators after the vaginal tissue has healed sufficiently. Exercises can be done at any time.
Note: NEVER use a vaginal product that contains estrogen as it could affect your cancer or your treatment.
Moisturizers
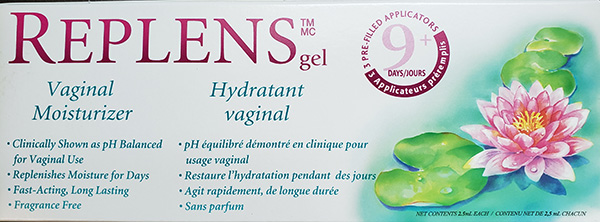 Vaginal moisturizers are needed by all young women who have been put into temporary or permanent menopause by their cancer treatment, whether or not they are sexually active. Just like using a moisturizer to help dry hands, a vaginal moisturizer helps to keep vaginal tissue moisturized and plumped up. Vaginal moisturizer comes in several forms such as creams with or without applicators, and suppositories. Effective varieties available over the counter in Canada include ReplensTM, RepagynTM and GynatrofTM. You may have to try a few different ones before finding one that works best for you. Use as directed by the package instructions. It’s never too late to start moisturizing, but you can avoid symptoms such as vaginal dryness, itching and painful intercourse if you start moisturizing as soon as your periods stop. Proactively applying moisturizer even once a week prevents deterioration that will necessitate nightly use for several weeks. If dryness has already set in when you start using these products they will often seem runny and messy (‘goopy’) but don’t quit! With consistent use, the dry, dead tissue that has been lining your vagina will slough off leaving healthier tissue underneath that can hang on to the moisturizer, resulting in less of it dripping out.
Vaginal moisturizers are needed by all young women who have been put into temporary or permanent menopause by their cancer treatment, whether or not they are sexually active. Just like using a moisturizer to help dry hands, a vaginal moisturizer helps to keep vaginal tissue moisturized and plumped up. Vaginal moisturizer comes in several forms such as creams with or without applicators, and suppositories. Effective varieties available over the counter in Canada include ReplensTM, RepagynTM and GynatrofTM. You may have to try a few different ones before finding one that works best for you. Use as directed by the package instructions. It’s never too late to start moisturizing, but you can avoid symptoms such as vaginal dryness, itching and painful intercourse if you start moisturizing as soon as your periods stop. Proactively applying moisturizer even once a week prevents deterioration that will necessitate nightly use for several weeks. If dryness has already set in when you start using these products they will often seem runny and messy (‘goopy’) but don’t quit! With consistent use, the dry, dead tissue that has been lining your vagina will slough off leaving healthier tissue underneath that can hang on to the moisturizer, resulting in less of it dripping out.
Lubricants
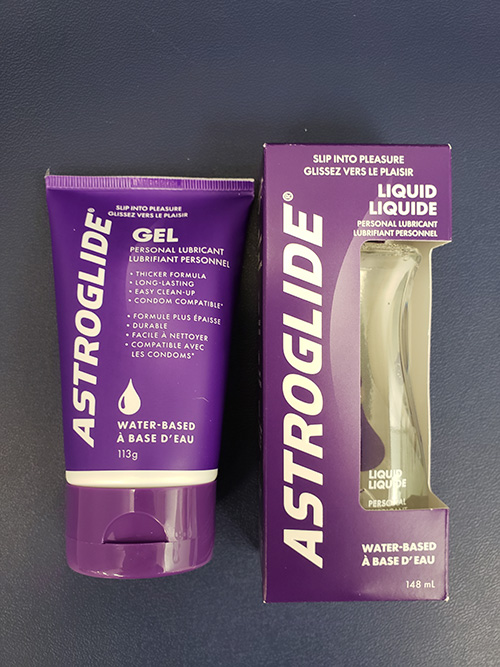
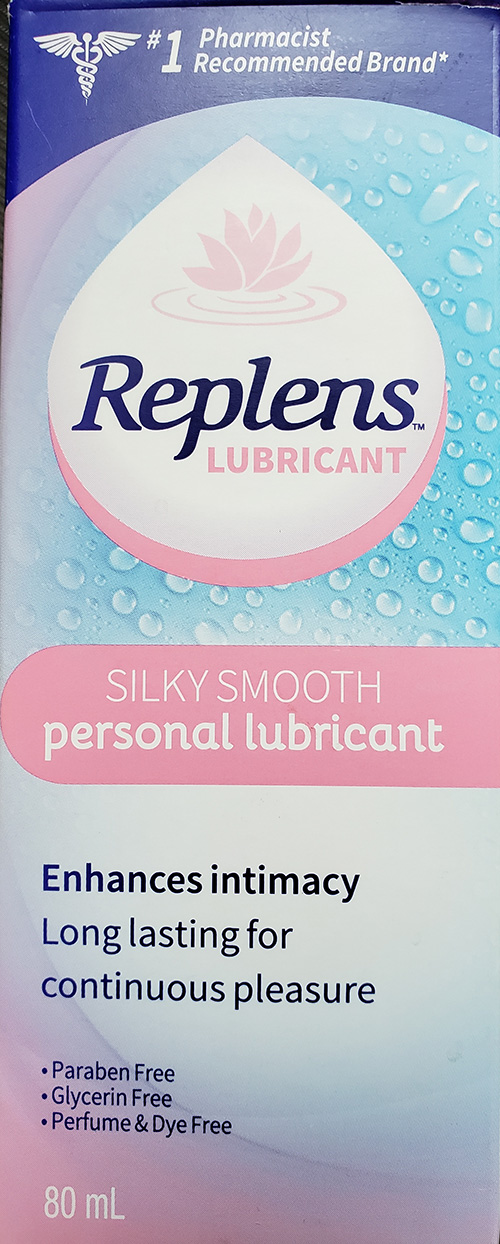 Vaginal lubricants make penetration easier and decrease friction during sexual intercourse or insertion of dilators (see below). Many women use these products even if they are not yet in menopause. Women in menopause should only use a water-based lubricant such as K-YTM or AstroglideTM. Lubricants that are flavoured or give a heating sensation are very irritating to dry tissues, so never use them. Water-based lubricants are best because they are thin and easily discharged from the vagina.
Vaginal lubricants make penetration easier and decrease friction during sexual intercourse or insertion of dilators (see below). Many women use these products even if they are not yet in menopause. Women in menopause should only use a water-based lubricant such as K-YTM or AstroglideTM. Lubricants that are flavoured or give a heating sensation are very irritating to dry tissues, so never use them. Water-based lubricants are best because they are thin and easily discharged from the vagina.
Note: Lubricants do not moisturize the vagina. They dry out within a short period of time, and can even feel painful when applied to dry or cracked vaginal tissue.
Dilator Kit
Part of the process of vaginal atrophy is the shrinkage in length and width of the vaginal walls, particularly the opening of the vagina. Once moisture is replenished in your vagina you should start using the dilator kit. It contains silicone dilators of various lengths and widths. Using a lubricant, start with the largest size you can insert without any pain.
With routine use, the vagina will stretch, open and lengthen over time. Dilators are particularly important when a woman is not having regular vaginal intercourse.
Pelvic Floor Exercises
 These exercises (also known as Kegels) are often practiced by women before childbirth or by women prone to stress incontinence (a bladder that leaks under stress such as sneezing). Exercising the pelvic floor muscles helps to bring extra circulation to the vagina and this increased blood flow heals atrophying structures, with the added bonus of intensifying orgasm.
These exercises (also known as Kegels) are often practiced by women before childbirth or by women prone to stress incontinence (a bladder that leaks under stress such as sneezing). Exercising the pelvic floor muscles helps to bring extra circulation to the vagina and this increased blood flow heals atrophying structures, with the added bonus of intensifying orgasm.
Start with an empty bladder. You may do the exercises standing, sitting or lying down. Identify your pelvic muscles by inserting two fingers into your vagina and squeezing the muscles around your fingers. The sensation is similar to stopping urination in the middle. Do the exercise by contracting these muscles and holding for five seconds, then completely relax for five seconds. Repeat 10 – 15 times. Over time, as your muscles get stronger, increase the length of time you are squeezing to 10 seconds. You will start to notice an improvement in stretch and function of your vagina.
Additional Measures Available

Vibrator
If you feel comfortable using dilators, you may add the benefit of a vibrator. Consider it an “internal massage” to bring increased circulation to the vaginal tissues.
Laser treatment
Laser treatment is the use of a specialized laser to cut through any scarring that may have taken place while vaginal atrophy has been occurring. This is performed in a hospital or private clinic by a gynecologist trained in the procedure. Women who continue to have symptoms of vaginal dryness, with no improvement after trying the other ‘tools’ in their kit for several months, may wish to ask their doctor for a referral to a centre where this is done to discuss the benefits and possible risks. There is a charge for this treatment as it is not covered by the Ontario Ministry of Health.
Every woman’s individual needs will require slightly different interventions. Some women will only need to regularly use a vaginal moisturizer and add a lubricant when having sexual intercourse. Others will need to employ additional methods discussed in this guide. Professional help may be necessary to design an appropriate treatment regimen if getting started on one’s own is too painful or there is no sign of improvement after several weeks.
Finally, please don’t hesitate to discuss any of this with your medical oncologist, family doctor or breast centre nurse!





