Simulation
In October 2016, the Sunnybrook Canadian Simulation Centre (SCSC) received accreditation from the Royal College of Physicians and Surgeons of Canada for the next five years. We are the first centre in Ontario and the third in Canada to be re-accredited by the Royal College.
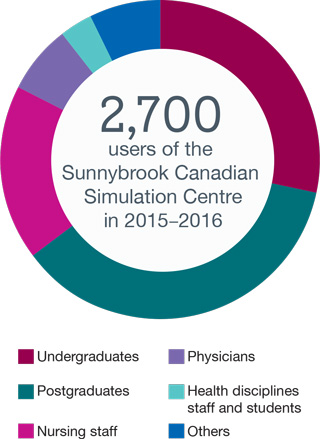
We increased learner participation by 28% this year, surpassing our target by 26%. The simulation programs explored opportunities to support corrective action and addictive training, specifically for practice re-entry and competency assessment through simulation.
This fall, the SCSC and trauma centre received the Toronto Police Traffic Services Appreciation Award in recognition of their collaboration and support in the development of the Police Officer’s Guide to the Trauma Room. The program combines an in-class session with instructional videos to help new officers become familiar with the trauma environment and members of the trauma team. The first of its kind, this orientation program was delivered at police headquarters to all new officers assigned to the hospital. Following the successful implementation of this guide, the Toronto Police Services is recommending that a general version be provided to other provincial police services.

The Toronto Police Services recognizes the Sunnybrook Canadian Simulation Centre and trauma centre with a special award. (left to right) Inspector Andrew Noorie, Debra Carew, Constable Paul Breeze, Sharon Ramagnano, Dr. Avery Nathens, Dr. Ari Zaretsky, Agnes Ryzynski, Dr. Luis Da Luz. [Photo: Doug Nicholson.]

Simulation Committee Co-Chairs L to R: Agnes Ryzynski, Jordan Tarshis and Susan DeSousa.
Below are the initiatives that the Simulation Committee undertook this year.
National Surgical Quality Improvement Program (NSQIP) data indicated that Sunnybrook’s performance on catheter-associated urinary tract infections (CAUTI) was suboptimal. Consequently, Sunnybrook set a target to decrease CAUTI incidence by 60% by April 1, 2016. A strengths, weaknesses, opportunities and threats analysis was conducted, which highlighted an education gap concerning urinary catheter indication, insertion, follow up and discontinuation.
The aim of the course was to create a comprehensive educational intervention that encompasses gap analysis, sound instructional design and impact measurement to facilitate the corporate objective of reducing CAUTI by 60% by April 1, 2016. Further analysis indicated that the most significant learning gap was within the medical student population. The following educational interventions were implemented as a mandatory session for all Sunnybrook medical students during their surgery rotation:
- E-module and video
- Simulation including education, demonstration and 60 to 90 minutes of hands-on practice
- Assessment: 100% score on procedural checklist completed in Simulation Centre
Historically, there was an assumption that the current medical curriculum addressed this learning need during “Surgery Boot Camp”. Learners, however, demonstrated significant gaps in catheter indication and insertion procedure during their first catheter insertion.
After one-on-one learning sessions with an expert facilitator, learners were able to perform and demonstrate the correct procedure, showing an increase from 60% to 100% completion of the correct checklist steps.
The current surgery rotations are not sufficient for students to acquire the proper technique to place urinary catheters safely in patients. During the initial insertion learners indicated that they did not feel prepared or confident to insert urinary catheters on real patients. After reviewing the video and e-module and completing the simulation course, learners expressed their increased confidence and preparedness in performing the procedure on patients. Learners found the simulation course particularly helpful for a number of reasons, including:
- Opportunity to practice good hand hygiene and learn how to maintain a sterile field
- Availability of male and female models for practice
- Good student to instructor ratio
- Accuracy of simulation models and feedback.
With subsequent sessions we will be in a position to collect additional data to further assess the impact of this project on outcome. The evaluation strategy includes the following components:
- A pre-and post-training survey
- Assessment by the expert instructor using a procedural checklist while performing the skill
- Evaluation of hospital CAUTI rates before and after simulation training program
- Outcomes assessment against the NSQIP benchmark
Advance Care Planning (ACP) conversations are used to learn about a person’s values, beliefs and wishes related to their future health care. These conversations can occur at any stage of a person’s life, whether they are healthy or have a serious illness. The outcomes of these conversations can then be used to inform goals of care (GOC) discussions when treatment or care decisions are made. Improving communication skills in ACP and GOC conversations will lead to enhanced patient-centered care and greater satisfaction with care.
The ACP simulation program is a comprehensive interprofessional education initiative to build skills and confidence for all Sunnybrook staff to initiate quality of dying conversations. The goal of this corporate initiative and the broader Quality Dying Initiative is to support physicians in initiating conversations with patients and family members around illness understanding. The SCSC initiated the first ACP simulation program, which was launched during National ACP Week with great uptake. Participants commented that this was an extremely valuable resource and experience. Their feedback also demonstrated a demand for more simulation programs that extend to patients and families. Our next step will be to expand the program to encompass regular simulations starting with oncology and general internal medicine.
By the end of the ACP simulation program participants will be able to:
- Identify and clarify the role of the substitute decision maker
- Highlight the importance of person-centred conversations and best approaches
- Demonstrate continuum of conversation between ACP and GOC, as well as its iterative nature
The management of violent outpatient psychiatric patients was an identified gap that posed physical and psychological risk to staff. An interprofessional curriculum was developed for psychiatric nurses, staff psychiatrists and hospital security personnel. We provided a simulation-based training course, which received the Award for Most Outstanding Continuing Education Activity in Psychiatry in Canada from the Council of Psychiatric Continuing Education.
Sunnybrook started a new initiative to involve real Sunnybrook patients in education activities at the hospital. The goal of the initiative is to use invaluable real patient insight to improve the experience for all Sunnybrook patients. The SCSC was approached by senior leadership to create the first program involving patients in education at Sunnybrook. We incorporated this initiative into the anesthesia clerkship simulation curriculum, specifically in the exit day pre-op scenario.
In this scenario a Sunnybrook patient volunteer interacts with medical students during a pre-op assessment interview along with a standardized patient. The patient volunteer plays the sister of the standardized patient who is attending the pre-op clinic prior to surgery. At the end of the pre-op station, the patient volunteer is given the opportunity to speak directly to the students regarding her experience as a patient. The medical students are given the unique opportunity to hear and get feedback directly from a real patient on their interactions and ways to make the patient experience more comfortable and meaningful.
Feedback from the patient volunteers highlighted three key themes:
- Students need to simplify their language by avoiding medical jargon.
- Students need to improve their active listening skills.
- Students were highly confident and professional.
There was consensus among the medical students that the initiative contributed positively to their professional development by providing an opportunity to understand better the patient’s perspective. Based on feedback, 77% of students said this experience motivated them to change their practice, particularly with respect to body language, active listening, sensitivity, empathy and mindful communication.
Read about this initiative in the Jan 2016 issue of the Hospital News.
Watch a video showcasing this unique and innovative simulation experience.
The dialysis unit is being relocated from the main campus to another building where there will not be cardiac arrest teams. As such, automated electrical defibrillators (AED) were purchased for the new location. All nurses and dialysis physicians underwent interprofessional simulation training on this new equipment prior to the move to ensure patient safety at the new location. This course also provided the nurses and physicians with the necessary competencies to identify and treat deteriorating patients and operate an AED safely.
- To respond to emergency situations in a timely manner utilizing critical thinking skills
- To apply knowledge and skills related to basic cardiac life support with AED appropriately, within a non-threatening environment
- To communicate effectively and work collaboratively as a team
SCSC has partnered with the Emergency Preparedness Department and the CPR Executive Committee to develop and implement routine mock Code Blue simulations throughout Bayview campus. The goal of these simulations is to improve the team's response time to first defibrillation to less than three minutes. By running simulations in real settings, team members will be able to improve their technical skills, strengthen team communication and enhance situational awareness. These simulations will be conducted on an ongoing basis.
Our future initiatives include:
- Increase number of teachers and learners
- Acquire new simulation equipment to expand access and opportunities for learners
- Expand quality improvement initiatives via skill acquisition, practice and impact measurement
- Continue to expand national and international leadership