
Breaching the blood-brain barrier: why it matters
November 8, 2015
Donate now
Thank you for your generosity.
Your donation is helping to invent
the future of health care.
Sunnybrook scientists made history this week as they used focused ultrasound to non-invasively breach the blood-brain barrier in an effort to more effectively deliver chemotherapy into the brain tumour of a patient.
What is the ‘blood brain barrier’ (BBB)?
Each person has a protective blood barrier lining the blood vessels in the brain to restrict the passage of large toxic substances from the bloodstream into the brain.
You can imagine the barrier acting like plastic wrap around the small blood vessels. In most areas of the body, there is no plastic wrap and whatever is in the bloodstream can get into the various tissues of the body, such as muscle, etc.
In the brain, all of the blood vessels have this “plastic wrap” around them that only allows very select molecules to get through.
Why would anyone want to “break” it?
The BBB has been a persistent obstacle to delivering valuable medication therapies to treat diseases of the brain such as tumours and various types of neurological disorders because of its “plastic wrap” layer around the blood vessels.
Some medications can get through this BBB but it can vary from zero percent to a small amount. For example, some chemotherapy has up to a 20 per cent chance of reaching these parts of the brain because of the BBB.
Researchers are hoping that by temporarily and safely opening this barrier in a patient to deliver medication directly to the brain tumour, it may potentially mean providing more targeted treatment in the future, which they think will require less medication, leave fewer side effects and improve quality of life.
What happened at Sunnybrook?
Sunnybrook scientists made history as they used focused ultrasound to non-invasively breach the blood-brain barrier in an attempt to more effectively deliver chemotherapy into the brain tumour of a patient.
They essentially poked holes in the “plastic wrap” and allowed the various chemicals that they want delivered to the brain to get into the brain.
View video about this world-first and meet the patient:
How did they do this?
On the first day, the patient received a small dose of chemotherapy that was slowly infused into her bloodstream through a drip IV in her arm.

She was then taken to an MRI Suite where she was prepped for the focused ultrasound procedure. A head frame was screwed to her skull and she laid down on the MRI bed where the head frame was connected to a “helmet” that is part of Insightec’s Exablate Neuro System.

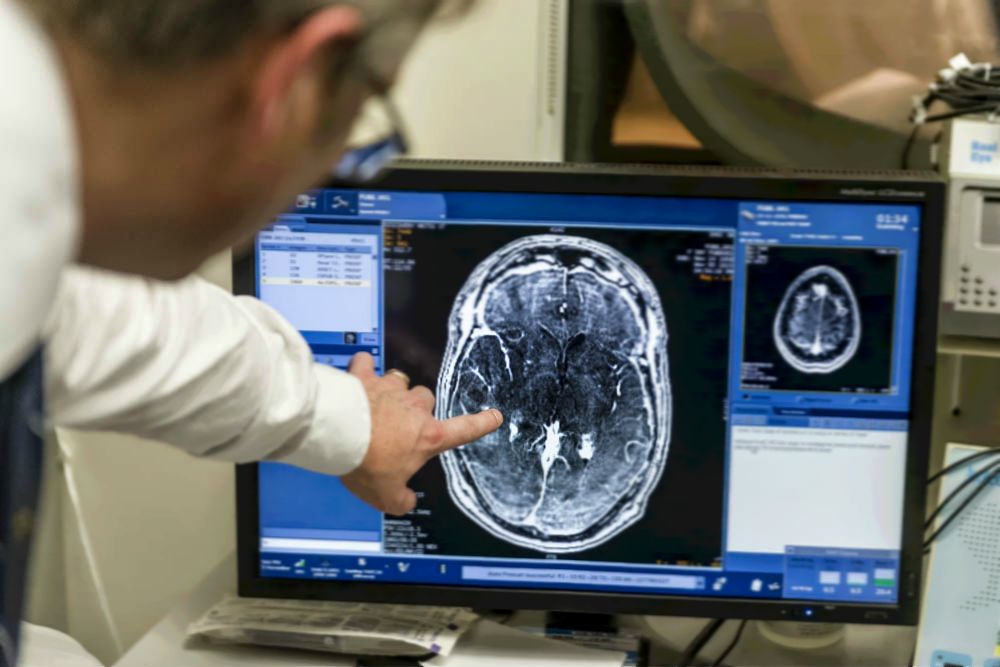
A number of standard MRI scans were initially done to help the researchers locate positions and plans of where they needed to go.

The researchers administered microscopic bubbles into the patient's bloodstream through an IV. The microbubbles are smaller than red blood cells and pass harmlessly through the circulation. Once ready, the researchers used state-of-the-art MRI-guided focused low-intensity ultrasound (sound waves) to target blood vessels in the BBB area near the tumour.

How does the ultrasound work to open the BBB?
The sound waves repeatedly compressed and expanded the microbubbles, which caused them to vibrate and loosen tight junctions of the cells comprising the BBB. Once the barrier was opened, the chemotherapy flowed through and deposited into the targeted regions.
Can you see it?
You cannot see the opening of the BBB with the human eye. With the use of a contrast dye that was injected, the researchers were able to see on the MR scans that the BBB opened, and believe the chemotherapy flowed in to the targeted part of the brain tumour.
Why did she have surgery if the idea was to breach the BBB non-invasively?
The participants in the trial are those already scheduled for traditional neurosurgery to remove parts of their brain tumour.

The opening of the BBB using the focused ultrasound the day before surgery was non-invasive and was successful at breaching the barrier.
How long does the BBB stay open and how do they know the BBB is closing?
The BBB remains open for up to 12 hours. The researchers know the BBB is closing by the disappearance of contrast enhancer.
Is dosage of chemotherapy the same as that given during a regular treatment of it?
No. This is a potentially novel use for this chemotherapy.
Isn’t it dangerous to inject bubbles into the brain? Couldn’t it cause a stroke?
These bubbles are so tiny they’re microscopic and are smaller than red blood cells. They pass harmlessly in the blood through the circulation system. Once in the area they want them, the researchers use the focused ultrasound to activate them to open the BBB.
What are the risks?
All procedures carry risk. There is a chance of a brain bleed and therefore the patient is closely monitored by a large interdisciplinary group including neurosurgeons, an anesthetist, radiologist, oncologist and physicist. This research is carried out within a hospital environment with access to care and leading brain health specialists.
If found effective, who will this approach help?
Breaching this barrier opens up a new frontier in treating the brain. The success of this research opens up the potential for delivering drug therapies to parts of the brain protected by the BBB, including researching treatments for patients with various kinds of brain tumours, Alzheimer’s disease, and some psychiatric conditions.
Implications of this research and information about the trial
While this breakthrough opens up potential in the future for delivering drug therapies to parts of the brain protected by the blood brain barrier (BBB), please note that the patients (known as research participants) in this clinical trial will not benefit from this procedure (the opening of the BBB and any chemotherapy that gets through).
These research participants will undergo needed surgery to remove much of their brain tumour the next day. Therefore any chemotherapy that did potentially get through to the brain tumour will also be removed.
The point of this trial is to test for the feasibility, safety and proof of concept of using MR-guided focused ultrasound to temporarily open the BBB to get chemotherapy across into the brain tumour directly.
This case was the first of up to 10 participants in this study; all of the participants will be those who are already scheduled for traditional neurosurgery to remove parts of their brain tumour.
Enrolment is currently limited to Canadian residents only, due to the inpatient surgical procedure.
For more information on this procedure & potential future applications for this research, please see our press release, and the Focused Ultrasound Foundation:
We are fortunate at Sunnybrook to have a large interdisciplinary group of physicists, radiologists, neurosurgeons and oncologists that can work together and push this trial forward.







