Abstracts
Dynamic Duos
Spinal metastasis, or cancer that has spread to the spine, occurs in 30% to 50% of all cancer patients, and puts them at increased risk of spinal fracture. Photodynamic therapy (PDT) is a minimally invasive procedure that has been shown to destroy tumours and improve the structure and strength of the spine in the short term. It uses a drug called a photosensitizer that is activated by light. When the drug is exposed to a certain wavelength of light, it makes an oxygen molecule that kills nearby cells.
Dr. Cari Whyne, director of the Holland Bone and Joint Research Program at Sunnybrook Research Institute, led a study aimed at assessing the effect of PDT after a longer time period, alone and combined with prior bisphosphonate or radiation treatment. She found preclinical models treated with a combination of PDT and bisphosphonates (drugs that prevent loss of bone mass) showed enhanced bone formation and structural integrity six weeks after treatment, compared with untreated controls and those who received one type of therapy. Radiation combined with PDT yielded the next best improvement in bone architecture. The findings highlight the promise of PDT as an adjunct treatment for spinal metastasis.
Choosing a Prostate Cancer Treatment? Know All of the Risks
Incontinence and erectile dysfunction are two well-studied adverse effects of prostate cancer treatment, but there are other potential problems to consider.
Dr. Robert Nam, a researcher in the Odette Cancer Research Program at Sunnybrook Research Institute, led the first study to turn the spotlight on other complications after radiotherapy and surgery for prostate cancer.
The study, published in Lancet Oncology, looked at data of more than 32,000 men in Ontario who underwent treatment for prostate cancer between 2002 and 2009. Nam and colleagues found the five-year cumulative risk of complications, including hospital admission, urological procedures, rectal or anal procedures, open surgeries and secondary cancers, was significantly higher among those who had treatment compared with matched controls with no history of prostate cancer. They also found radiation was associated with higher incidence of all complications except urological procedures, compared with those who had surgery.
These findings can help doctors bring to bear the complications of therapy—all of them—on their discussions with patients about treatment options.
Going Back to Work After a Burn Injury
Research shows most burn injuries occur in people aged 20 to 44 years—prime working years. Although returning to work is an important goal for these individuals, there are significant challenges to doing so, including pain, disruption in sleep patterns and emotional distress. Moreover, an inability to return to work following a burn has been shown to worsen anxiety, resulting in poorer quality of life.
Clinical guidelines for initial recovery and rehabilitation after a burn injury do not address issues regarding work re-entry. To fill this gap, Dr. Manuel Gomez, director of the St. John’s Rehab Research Program at Sunnybrook Research Institute, and colleagues developed the first clinical practice guideline aimed at helping health care teams, patients and employers to assess a person’s ability to return to work after a severe burn.
The purpose of the guideline, published in Burns, is to improve burn survivors’ employment outcomes by promoting a systematic approach to vocational evaluation. The authors note the target population is people aged 20 to 65 years; the target users includes these people, along with health and vocational professionals, and employers. The guidelines might also be of use to educators, insurers, family members and policy makers.
Flu Worse Than Flu Shot
Each year, the urging: get your flu shot! It sits against a wall of statistics: seasonal influenza causes 3 to 5 million cases of severe illness and 250,000 to 500,00 deaths worldwide—every year. In Canada, between 2,000 and 8,000 Canadians die of flu and its complications annually. Research shows that in healthy adults, vaccination cuts infection risk by upwards of 60%.
Research also shows that Guillain-Barré syndrome, an acute autoimmune disorder whose effects can be life-threatening, has been linked to flu vaccination, which may be a barrier to achieving high vaccination coverage. It has also, however, been linked to influenza infection itself.
Dr. Jeff Kwong, a clinician-scientist in the Veterans Research Program at Sunnybrook Research Institute, led a study to get some clarity on the matter. The study found that the syndrome is associated with exposure to the vaccine and the flu illness. Critically, it found that the risk of Guillain-Barré syndrome after influenza illness was greater than after flu vaccination. The authors noted it is important that patients be informed of the risks, in context, of Guillain-Barré syndrome from both the flu vaccine and the flu.
A Fair Comparison
Computerized tomography (CT) uses X-rays to make cross-sectional pictures of the body. It is a useful diagnostic tool; however, scans are costly. As with all health care resources, practitioners must balance prudent use of finite means against provision of the best care possible.
Dr. Michael Schull, a clinician-scientist in the Tory Trauma Research Program at Sunnybrook Research Institute, and colleagues compared use of CT in emergency departments in the U.S. and Ontario, Canada between 2003 and 2008. They focused on four common conditions: abdominal pain, complex abdominal pain, headache, and chest pain or shortness of breath. The researchers found that in these cases, American emergency department clinicians used CT more often than did those in Ontario. Moreover, rates of CT use increased in both regions, but they did so faster in the U.S. However, for patients with complex abdominal pain who were admitted to hospital, the proportional use of CT was nearly identical. The authors noted that these findings suggest the availability of CT in Ontario is not so limited that it prevents the most critically ill patients from receiving CT, but that further study is needed before such a conclusion can be made definitively.
Scalpel-Free, But Not Risk-Free
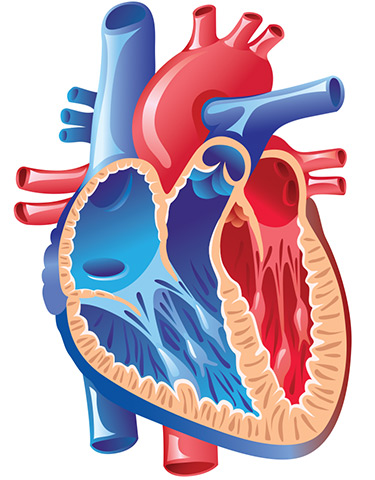
Aortic stenosis is narrowing of the aortic valve, which blocks blood flow from the heart to the body. Symptoms include chest pain, shortness of breath and fainting.
Transcatheter aortic valve implantation (TAVI) is a nonsurgical procedure in which doctors use catheters to implant a new valve over the existing one. It is offered to people who, due to other medical conditions or age, cannot tolerate surgery.
While uptake of TAVI has been rapid, the procedure is not without risk. Dr. Dennis Ko, a clinician-scientist at Sunnybrook Research Institute, led a study to quantify the adverse effects associated with TAVI, and to evaluate whether the type of valve used and the route of implantation are linked to differences in adverse outcomes.
The most common negative outcome was a problem with the heart’s electrical system, which requires a permanent pacemaker. Vascular complications and acute kidney failure requiring replacement therapy followed. The authors noted that the type of valve and route of implantation also affected the rates of complications.
Results of the review, published in the Annals of Internal Medicine, may help clinicians and policy makers to understand better the risk-benefit profile associated with the procedure.