Safe use of opioid pain medicine after surgery / trauma
Information for patients and families
Introduction
You have been prescribed an opioid pain medicine that is also known as a narcotic. This guide reviews some important safety information about opioids.
Patients, family, friends, and caregivers can play an important role in the safe use of these medicines. Share this information with them.
Click each section below to read more, or download a PDF version of this guide ![]()
» Opioids and your pain control
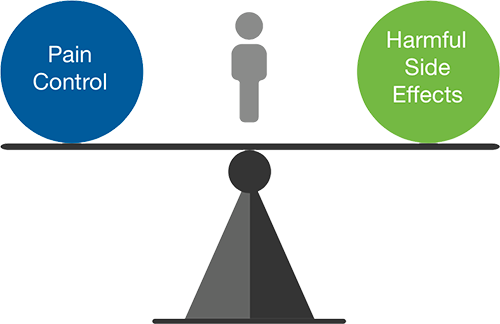
When you take opioid medication there is a balance between pain control and harmful side effects. This is why it is important to make sure you take the medication as directed.
Pain management is important to your wellbeing. Opioids will lower your pain and help you do your day to day activities with less pain. They will NOT lower your pain to zero.
Be sure that you understand your plan for pain control and work closely with your doctor if you need opioids for more than 1 to 2 weeks.
» What are the possible risks of taking opioids?
 Many people use opioids without problems. However, there are risks of serious problems, including overdose (taking too much) and addiction.
Many people use opioids without problems. However, there are risks of serious problems, including overdose (taking too much) and addiction.- It is important to follow the instructions on the prescription. Use the lowest possible dose for the shortest possible time. Be aware of signs (listed on next page) that you are getting too much opioid.
- Because opioids make you sleepy, avoid alcohol and sedatives such as sleeping pills.
» What are the common side effects?
- Feeling tired or sleepy
- Constipation
- Nausea
- Dry mouth
- Itchiness
- Sweating
- Dizziness
You should not drive or operate machinery while taking opioids.
» Remember, it’s important to:
- Never share your opioid medicine with anyone else.
- Store your opioid medicine in a safe place; out of reach and out of sight of children, teens and pets.
- Get rid of your opioids as soon as you don’t need them anymore. Do not throw them in the toilet or throw them out in the garbage. Take unused medicine back to a pharmacy for safe disposal.
- The Sunnybrook Ambulatory pharmacy on M1 in the main lobby will accept your unused medicine.
- For other locations that accept returns: 1-844-535-8889 or visit healthsteward.ca
 » What are the signs of overdose?
» What are the signs of overdose?
Stop taking the drug and get immediate medical help if you feel the following:
- Severe dizziness
- Inability to stay awake
- Hallucinations, such as seeing or hearing things which are not there
- Heavy or unusual snoring
- Shallow or slow breathing rate
Your family member or caregiver needs to call 911 right away if:
- You can’t speak clearly when you wake up
- You can’t be woken up
- Your lips or fingernails are blue or purple
- You are making unusual heavy snoring, gasping, gurgling or snorting sounds while sleeping
» Pain management guide
| How intense is my pain? | What can I take to feel better? |
|---|---|
|
Non-medication therapies + Non-opioid, oral medications |
|
Non-medication therapies + Non-opioid, oral medications |
|
Non-medication therapies + Around-the-clock non-opioid medications + Short-acting opioids (for a few days) |
» What are the most common pain control therapies and medications?
|
Mild pain
|
Non-medication therapies | |
| Therapy | Description | |
| Self-care | Ice, elevation, and rest | |
| Complementary therapies | Meditation, acupuncture, massage, and music | |
| Rehabilitation therapies | Occupational and physical therapy | |
| Exercise | Stretching, walking and mild exercise | |
|
Mild to moderate pain
|
Non-opioid, oral medications | |
| Medication | Common side effects | |
| Acetaminophen (Tylenol*): Decreases pain and fever |
Nausea, vomiting, headache, and insomnia Liver damage may occur if you take more than the recommended dose |
|
|
Non-steroidal anti-inflammatory drugs (NSAIDs): Decrease swelling and fever • Naproxen (Aleve) |
Upset stomach: Stomach bleeding or ulcers, heart attack, and stroke | |
|
Nerve pain medications: • Gabapentin |
Dizziness, drowsiness, swelling in the hands and feet, weight gain, and blurred vision | |
|
Muscle relaxants: • Robaxin (methocarbamol) |
Lightheadedness, dizziness, drowsiness and mild nausea | |
|
Severe pain
|
Opioids | |
| Medication | Common side effects** | |
| Opioids: Hydromorphone (Dilaudid) Morphine Oxycodone |
Dizziness, nausea (very common), headache, drowsiness, vomiting, dry mouth, itching, respiratory depression or very slow breathing, and constipation To prevent constipation, stool softeners or laxatives may be prescribed. Eating a high fiber diet, drinking lots of fluids and exercising daily may also help. Serious risks include misuse, abuse, addiction, overdose (taking too much of the medication), and death from suppressed breathing |
|
American College of Surgeons: facs.org/safepaincontrol
**Side effects reported in 3% or more of the patients in the study sample