Sunnybrook recruits leading neuroscientist in ophthalmology research
Dr. Carol Schuurmans had a pretty nice gig in Calgary. She was a tenured professor at the University of Calgary with an established and productive lab that she had built over 15 years. “I was not looking to leave Calgary,” says the Edmonton native.
An email from Dr. David Andrews, director of Biological Sciences at Sunnybrook Research Institute (SRI), changed all of that. At Andrews’ invitation, Schuurmans came to give a talk at SRI about her work. “I came and got really excited,” she says. “There’s good people [here], and the institute is fantastic.”
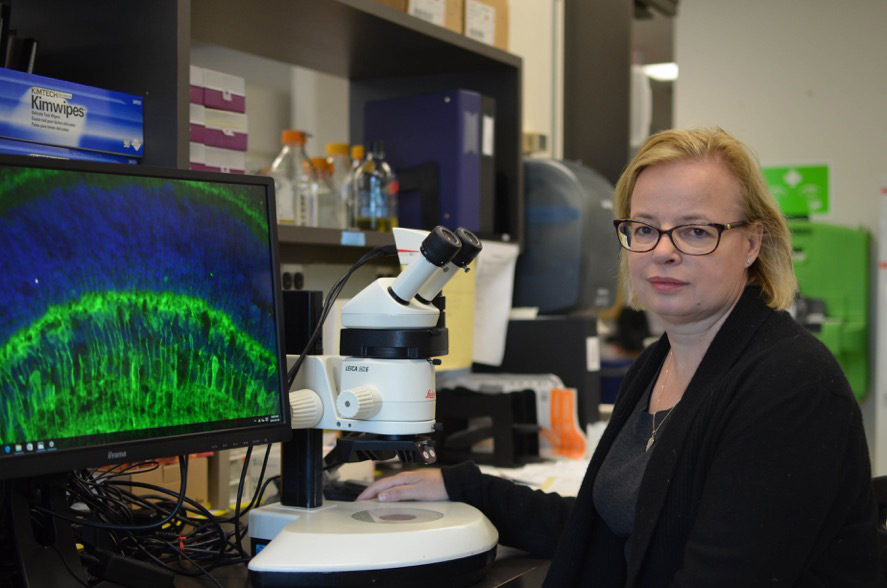
Ultimately, it was the combination of people and facilities that helped her realize that she could do things here that she couldn’t do in Calgary. This summer, Schuurmans relocated her lab to Toronto, where she is now the Dixon Family Chair in Ophthalmology Research and senior scientist in Biological Sciences at SRI.
As a neuroscientist, Schuurmans studies how neurons are generated in the developing nervous system. She is particularly interested in how different types of neurons form at distinct times in the developmental process and acquire their specialized functions. Her research focuses on two specific areas: the neocortex region of the brain and the retina.
The neocortex is the outermost layer of the brain. It serves as a good model for studying neurogenesis and cell fate determination because it has a layered structure. Each layer contains a distinct kind of neuron and is formed in a specific sequence. “How do you get different types of neurons born at different times?” says Schuurmans. By understanding how these cells are made in the developing brain, she hopes to be able to improve treatment for injuries and diseases of the central and peripheral nervous systems.
“From a translational perspective, we’re interested in cell repair,” she says. “We want to take our knowledge of how neurons are born normally in development and apply that to regenerative medicine.”
In one project, Schuurmans and her team are trying to grow glial cells in the lab. Glial cells support and protect neurons. When the nervous system sustains an injury these cells are activated to help make more neurons. Schuurmans thinks that if you could give lab-grown glial cells to patients with brain or spinal cord injuries, then the cells could boost our nervous system’s ability to repair itself.
Schuurmans is also looking at glial cells in the retina and their role in treating vision loss. She is focusing on a type of cell called Müller glia, which in frogs and fish become activated in response to retina damage. Once activated Müller glia become stem cells that can form retina cells and replace the cells that were destroyed in the injury. This regenerative capability enables fish and frogs to repair retina damage and maintain their vision. Mammals, on the other hand, have Müller glia but cannot turn them on efficiently. To tap into this potential source of regenerative cells, Schuurmans and her team are searching for ways to trigger Müller cells to switch into stem cells. As a first step, they have identified a gene that, when mutated, seems to play a role in activating these cells.
In a complementary approach, Schuurmans is using a novel genetic strategy to reprogram skin cells into retina cells that could be used to replace the cells that are lost in patients with degenerative eye disorders such as retinitis pigmentosa and age-related macular degeneration. If successful, then this strategy would get around one of the most pressing issues in the field—a safe and renewable source of cells for transplant. Her work thus far has focused on generating functional retina cells in a Petri dish. Preliminary work transplanting these cells into the retina of preclinical models has shown that the technique works, albeit at a very low efficiency.
“What we would like to do is inject our cells into the retina and see whether using [focused] ultrasound is a better way of getting the cells in,” says Schuurmans. To that end, she plans to begin working with senior scientists Drs. Isabelle Aubert and Kullervo Hynynen to explore how focused ultrasound can be used to open the blood-retina barrier and improve transplant efficiency.
Schuurmans says that the focused ultrasound expertise at SRI was a big reason why she decided to move to Toronto. She was also drawn by the good manufacturing practices facility that is part of the Centre for Research in Image-Guided Therapy at SRI and the opportunity to take part in clinical trials with experienced clinicians. “All of those things make it much easier if you’re trying to become translational,” she says. “It’s exciting because that’s ultimately where we want to go.”