American Asthma Foundation invests in novel asthma study
By Eleni Kanavas
The American Asthma Foundation (AAF) has awarded $150,000 to Dr. Daniel Dumont and his research team. Dumont and Drs. Paul Van Slyke and Annie Bourdeau will investigate a peptide mimetic called Vasculotide as a potential treatment for asthma.
Dumont, the director of molecular and cellular biology at Sunnybrook Research Institute, says, “This award is very important to our group as the funding provides a real boost to the research endeavour of the lab. It now provides support for my research team to look into the impact of Vasculotide in the early inflammatory response.” Dumont, who is also a professor at the University of Toronto, holds the Canada Research Chair in Angiogenic and Lymphangiogenic Signalling.
Vasculotide is a fully synthetic angiopoietin-ligand mimetic developed in Dumont’s lab that provides a unique access point into manipulating a particular cellular target that has been identified as dysfunctional in several different pathologies, including asthma.
“Work conducted in our lab and in the labs of several international collaborators demonstrates that Vasculotide, when used in a preclinical setting, provides an excellent therapeutic index that is well-tolerated and, thus far, seems to be free of detectable detrimental side effects,” says Van Slyke.
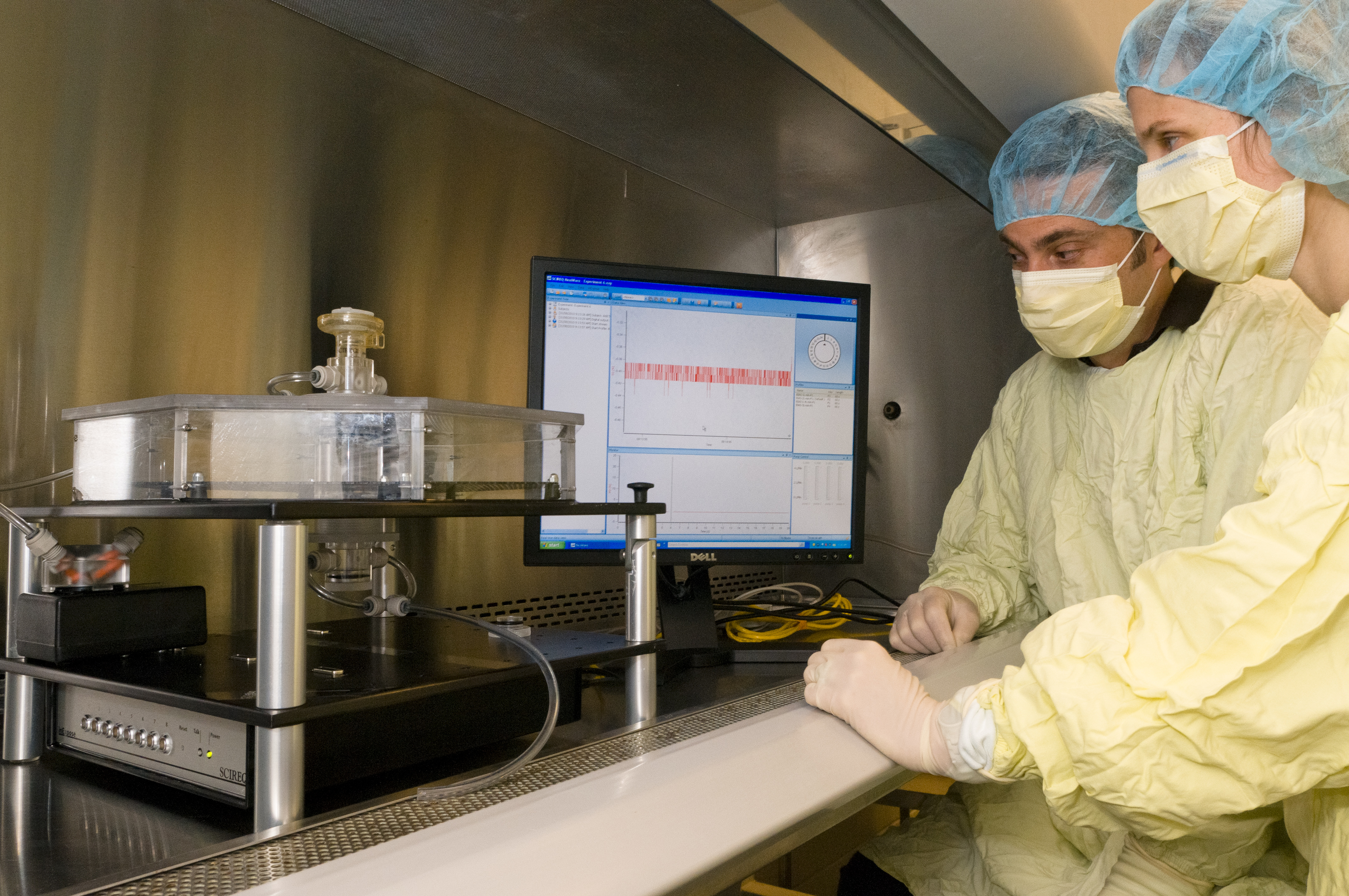
Bourdeau and Van Slyke will test Vasculotide’s ability to decrease the severity and long-term effects of asthma in mice by using the inExpose system, a bench-top inhalation exposure unit. The researchers will administer an asthma-inducing solution to two groups of animals, then inject Vasculotide in one group and compare their outcomes to the other (control) group. A total of 40 animals will be assessed in the experiment.
Vasculotide treatments will take about six months, followed by an additional six months for analysis to determine their impact on asthmatic symptoms. This work will be expanded and independently validated in collaboration with an asthma research core facility at the University of California in San Diego, says Van Slyke.
If the experiment ameliorates symptoms of the disease in mice, then it will provide Dumont's group with knowledge to develop Vasculotide further for dermatitis and rhinitis—two diseases that with asthma form the "atopic triad." Currently, Dumont's lab is also testing Vasculotide for diabetic wound-healing, artherosclerosis, ischemic limb disease and acute lung injury.
“Working with the AAF to assess the efficacy of a new drug candidate such as Vasculotide is very exciting, in particular given the rapidly increasing incidence of this disease,” says Van Slyke. “With the relative scarcity of research funding we are very pleased that the AAF shares our optimism for this study.”