Development and optimization of focal treatments
Treatments of bone metastases are designed to decrease pain, increase structural stability, improve mobility and control tumour growth. Treatments include systemic drugs [Bisphosphonates (BPs), Rank-L inhibitors (i.e. Denosumab) and chemotherapeutic agents (e.g. docetaxel)], focal treatments (i.e. spine stereotactic body radiotherapy [SBRT] and radiofrequency ablation [RFA]) and structural stabilization (i.e. cement augmentation or instrumentation). Our research has primarily focused on focal minimally invasive treatment modalities, including consideration of these treatments within a more comprehensive multimodal approach to the treatment of skeletal metastases.
Photodynamic therapy
Used clinically in the treatment of macular degeneration and light accessible cancers such as melanoma, Photodynamic Therapy (PDT) involves systemic administration of a photosensitizer that accumulates preferentially in target tissue and becomes activated by non-thermal light at a specific wavelength.
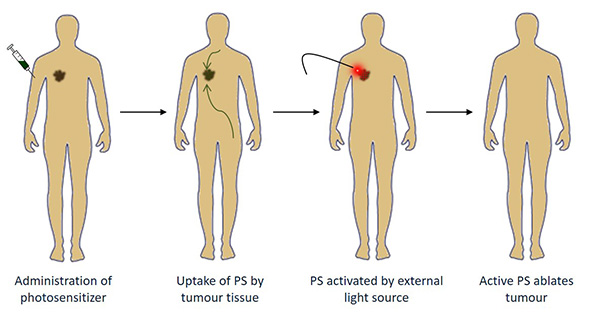
Click for plain-text version of infographic
- Administration of photosensitizer
- Uptake of PS by tumour tissue
- PS activated by external light source
- Active PS ablates tumour
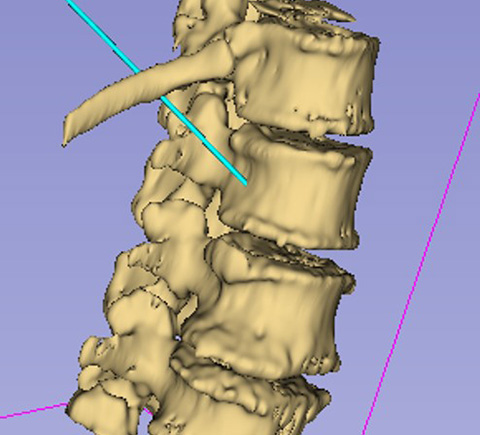
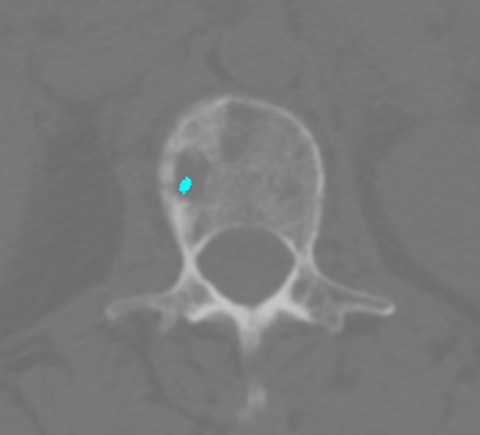
Activation of the photosensitizer in the presence of molecular oxygen leads to generation of highly reactive singlet oxygen, which causes tumor cell toxicity and tissue necrosis. A minimally invasive approach allows direct delivery of laser light to spinal lesions. Initial testing demonstrated the ability of PDT to ablate tumour tissue and augment the surrounding bone.
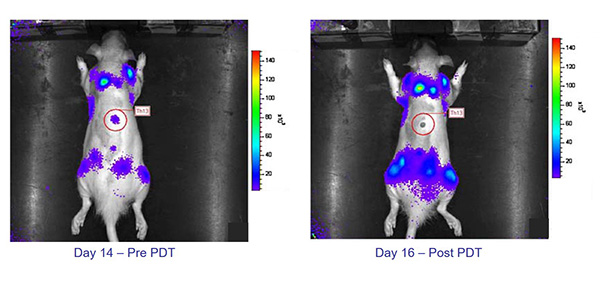 A reduction in bioluminescence demonstrates the impact of PDT on an osteolytic vertebral lesion.
A reduction in bioluminescence demonstrates the impact of PDT on an osteolytic vertebral lesion.
Click to view plain-text version of infographic
- Day 14 - Pre PDT
- Day 16 - Post PDT
A multimodal preclinical treatment study demonstrated the impact of PDT in conjunction with standard of care clinical treatments Bisphosphonates (BP) and Radiation therapy (RT). BP+PDT both destroyed the tumour and had the largest positive effect on bone, restoring bone volume fraction to non-tumour bearing control levels (with increased osteoid, woven bone, periosteal bone growth). An increase in bone volume was correlated to improved mechanical stability. Combined RT+PDT showed a similar effect on bone (lower magnitude).
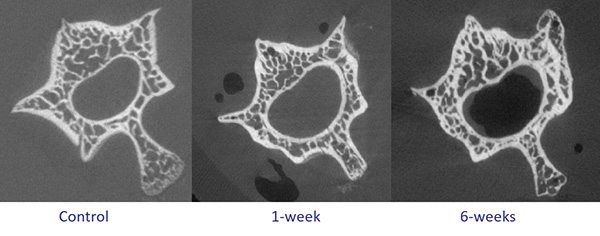 PDT leads to structural augmentation in the vertebrae, with increased bone deposition seen at one and six weeks post treatment.
PDT leads to structural augmentation in the vertebrae, with increased bone deposition seen at one and six weeks post treatment.
Click for plain-text version of infographic
- Control
- 1-week
- 6-weeks
Motivated by this promising preclinical work, a phase I clinical trial of PDT for spinal metastases has successfully been completed at Sunnybrook. Next steps will focus on treatment planning and running a Phase II clinical trial to quantify the direct impact of PDT on the vertebrae.
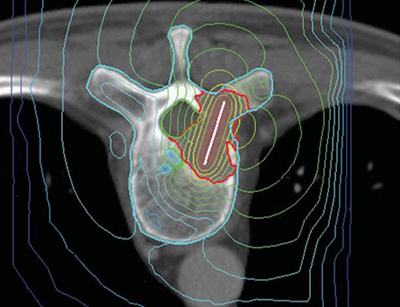

The clinical future of PDT.
Radiofrequency Ablation (RFA)
Radiofrequency (RF) refers to the electromagnetic spectrum covering the frequencies from 3 Hz to 300 GHz. In the context of tumour destruction, RF ablation induces ionic modulation leading to controlled heat production & local ablation of targeted tissue.
In collaboration with Baylis Medical (Mississauga, ON) we developed a novel bipolar internally cooled RF probe for the ablation of spinal metastases. The probe was designed to overcome previous limitations with RF of small and incomplete ablated regions, charring, boiling, iatrogenic injury, and difficulty completing the RF circuit in bone. Large lesions were ablated with RFA without damage to the neighbouring critical structures. Osteoclasts and tumour cells were also shown to be very susceptible to RFA but destruction of osteocytes was more limited (desirable for bone health).

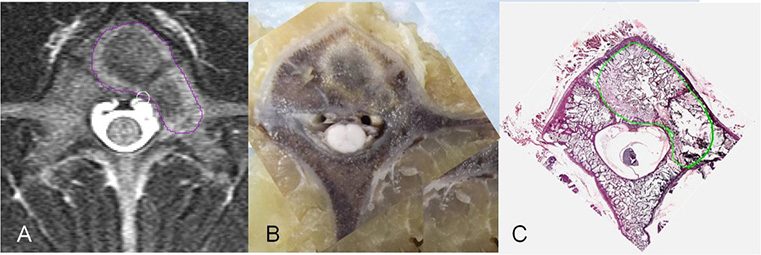
RFA of the spine: highlighted lesions are visualized on MR, optical and histology images.
The device was brought to first in human testing and ultimately became an FDA clinically approved device, Osteocool. With the sale of the Osteocool system to Medtronic, there is now worldwide clinical use of this device. We are currently developing a treatment planning and navigation system for RFA of spinal metastases with an integrated approach to enable multimodal treatment with SBRT.