Spine surgery outcomes and response shift
|
Change in rating of perceived QOL (observed) ↓ ↓ |
|
| Change explained by baseline and changes in health status (expected) | Discrepancy in QOL change (residual) ↓ |
| Response shift (measurement error) | |
This project is a prospective longitudinal study investigating spine surgery (discectomies, decompressions and fusions) outcomes with a special focus on the presence of response shift in disease and generic functional outcome measures. Response shift refers to the idea that Patient Reported Outcome Measures (PROMs) change over time and are influenced by many factors – physical, subject and evaluative.
The minimum important difference (MID) observed following spine surgery has varied drastically in the literature when considering PROMs. Here we are Investigating changes in patient's MID over recovery from spinal surgery and how cognitive appraisal processes are implicated in the change trajectories.
Measures:
- Rand-36 Physical and Mental Component Scores (PCS and MCS)
- Oswestry Disability Index (ODI)
- Pain Numeric Rating Scale Items (at rest, with activity, back and leg)
- PROMIS pain impact
- Global Assessment of Change (GAC) item
- The QOL Appraisal Profile - Standards of comparison domain
Among patients with different trajectories after surgery, the relationship between PROM change and appraisal change differs by group. Better, Worse, and Bouncer patients are focusing on different standards of comparison over time.
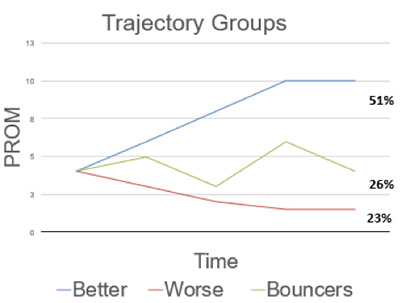
Factors affecting minimal important difference:
- Who you are asking (better or worse)
- How disabled are they at baseline
- When you are asking (time from surgery)
- What the patient is comparing themselves to
By identifying whether and which appraisal processes influence PROM trajectories, the present work provides potential avenues for clinical intervention to improve spine surgery outcomes.


