Energy to burn
Exercise on a hot day and, in addition to producing sweat, your skin will become flushed. That’s because as body temperature rises, blood vessels supplying the skin widen to bring more warm blood near the skin’s surface and release heat. The way in which our bodies regulate temperature is taken for granted by many, but not Dr. Chinthaka Heyn, a clinician-scientist at Sunnybrook Research Institute (SRI). To understand more about bioheat exchange, which is the study of heat transfer within living things, he has spent the last three years developing a way of measuring blood temperature using MRI.
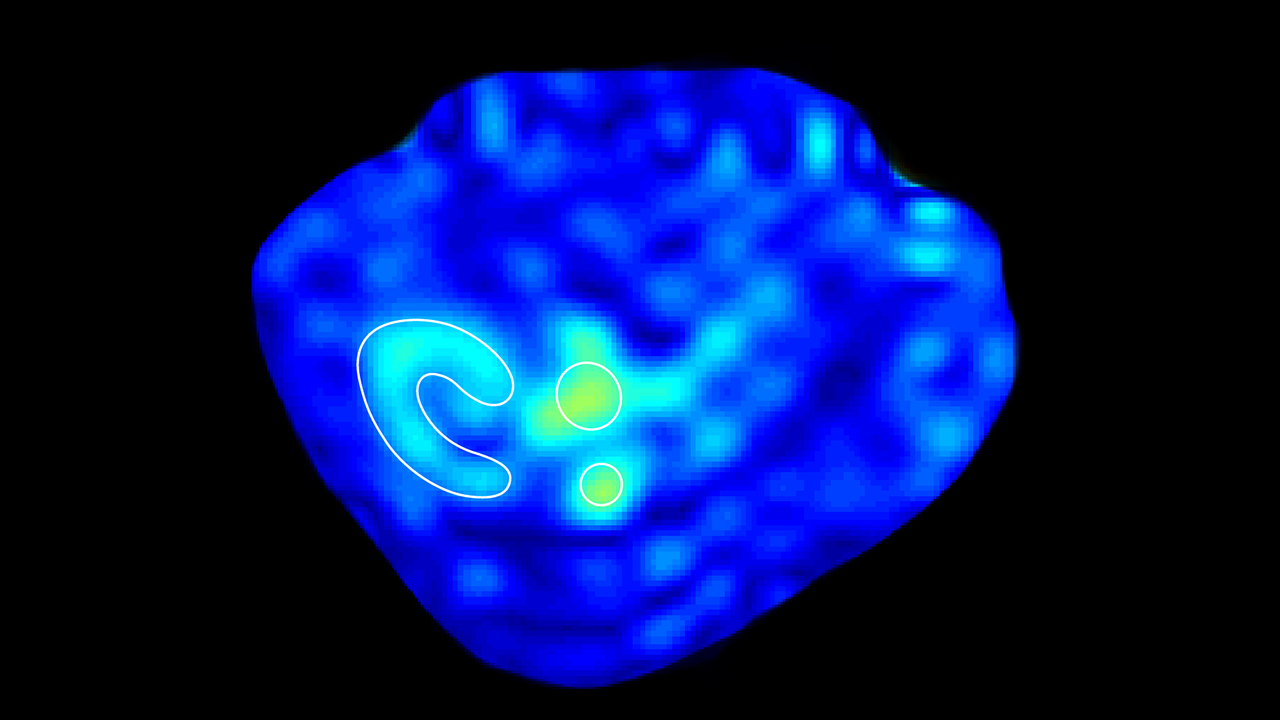
Heyn and colleagues from the Mouse Imaging Centre (MICe) in Toronto, Ont. were the first to measure the temperature of flowing blood noninvasively in mice. Using a novel MRI contrast agent that is temperature-sensitive, they found the temperature of the kidneys was significantly higher than that of the blood in the aorta, the largest artery in the body, and inferior vena cava, which carries blood into the heart. The study was published in NMR in Biomedicine.
Why should we care about the blood temperature of rodents? Heat, which derives from the breakdown of glucose, is a byproduct of metabolism and has to be removed from the body for cells to function properly. In 1948, an American neurologist named Harry Pennes sought to understand how this happens. Pennes did this by sticking probes into the forearms of subjects to measure temperature and blood flow. He discovered that blood flow cools the body much the same way that radiator fluid cools a car engine. The mathematical model that he created, known as the Pennes bioheat exchange model, describes the heat transfer relationship between arterial blood temperature and tissue.
Pennes’ model was widely adopted for its ease of use but has also been criticized because it doesn’t take into account the thermal effect of large vessels in the area being studied. “We know it’s not perfect, but we don’t have a better model. In order to show that that model is correct you have to make measurements. Now we’re able to make measurements and see where the model breaks down, make a better model. And that is the value of this work,” says Heyn. His study, which showed differences in arterial and kidney temperature, “are in line with what Pennes and others predicted” he says.
Assessing bioheat exchange by measuring blood temperature has broad applications, such as understanding how the body regulates temperature during exercise. There is growing evidence that increases in blood temperature during exercise lead to elevated brain temperature, which can cause fatigue and hinder athletic performance. Measuring blood and brain temperature could provide insight into this effect and lead to ways of enhancing achievement.
Heyn’s work also has implications for delivery of thermal therapies like focused ultrasound. The noninvasive technique, which has been approved to treat essential tremor, uterine fibroids and different types of cancer, uses heat to destroy tissue inside the body; but, notes Heyn, “in certain situations blood flow is significant and can remove a lot of the heat you’re depositing, making the therapy less effective.” When you know the relationship between arterial cooling of tissue and a heating process like focused ultrasound, you can model the energy required to transmit therapy appropriately, he says.
Bioheat exchange also provides a unique measure of tissue metabolism that complements measurements of glucose and oxygen consumption, which are shown by positron emission tomography, or PET. Unlike PET, however, studying bioheat exchange doesn’t require the use of ionizing radiation.
Next, Heyn will use bioheat exchange equations in work he is doing with SRI scientists Drs. Benjamin Goldstein, Simon Graham and Bradley MacIntosh and Dr. John Sled from MICe. They will examine brain metabolism in adolescents with bipolar disease. Looking at brain temperature, blood flow and blood temperature, they will search for evidence of problems with metabolism that may be behind the illness. “We’re embarking on these measurements of thermodynamics of the brain to see whether or not there are differences that we can detect very early, which could potentially be useful clinically; but, more important than making a diagnosis, it’s about understanding the pathophysiology of disease,” says Heyn.
Having validated Pennes’ model of bioheat transfer with his research, Heyn is excited by the possibilities. The contrast agent used in his thermometry studies has the same toxicity profile as dyes that are used routinely in people undergoing MRI. This means it holds the possibility of being used in humans—but clinical translation is not what inspires him most. “We didn’t do this set of experiments because we had a specific clinical application in mind. In fact, that wasn’t the reason at all. I think basic science work, even in the biomedical arena, should be done for the sole purpose of doing the science because you just never know what you’re going to find.”
This research was funded by the Canadian Institutes of Health Research.
Heyn CC et al. Magnetic resonance thermometry of flowing blood. NMR Biomed. 2017 Jul 7. doi: 10.1002/nbm.3772. This site uses a paywall.