Echoes of success
By Alisa Kim
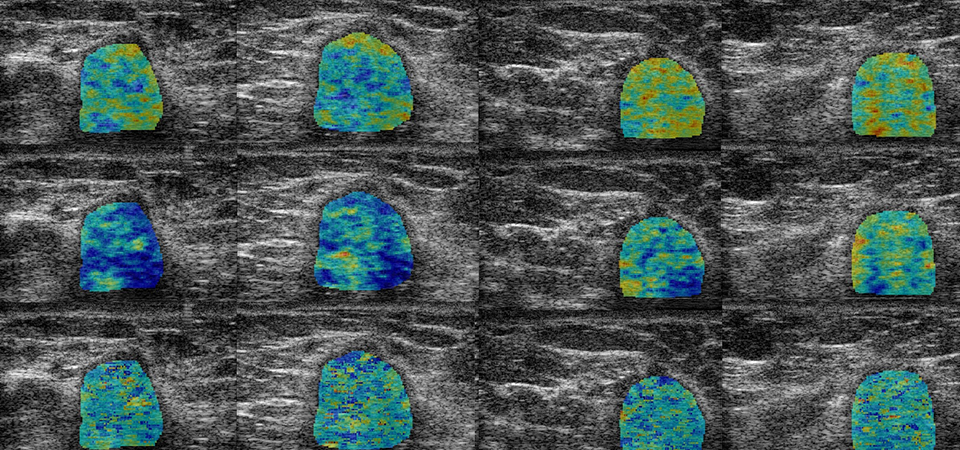
 Drs. Gregory Czarnota and Ali Sadeghi-Naini, scientists at SRI, have developed an ultrasound-based imaging technique that shows a patient’s response to chemotherapy very early on. Here, images of a breast tumour of a patient classified as a responder using their technique. The images were acquired before treatment and at various points after the start of chemotherapy.
Drs. Gregory Czarnota and Ali Sadeghi-Naini, scientists at SRI, have developed an ultrasound-based imaging technique that shows a patient’s response to chemotherapy very early on. Here, images of a breast tumour of a patient classified as a responder using their technique. The images were acquired before treatment and at various points after the start of chemotherapy. Cancer is abetted by inaction or the wrong action. In an ideal world, tumours would be detected early, patients would get treatment that works and the cancer would disappear. Sounds simple, right? Not so fast.
Take, for instance, locally advanced breast cancer (LABC), an aggressive subtype that afflicts up to 20% of women with breast cancer. A recent study shows that about 40% of women with LABC who have chemotherapy prior to surgery (neoadjuvant therapy, in medical parlance) respond poorly to the drugs.
“Right now when a patient receives chemotherapy, they typically have four to six months of therapy with no imaging or standardized clinical assessment of whether a tumour is responding,” says Dr. Gregory Czarnota, director of the Odette Cancer Research Program at Sunnybrook Research Institute (SRI) and chief of radiation oncology at Sunnybrook. “When someone starts on a course of chemotherapy, for the most part, they’re committed to it and have to finish it.”
Czarnota and his colleague, Dr. Ali Sadeghi-Naini, an imaging scientist at SRI, are working to infuse treatment with greater precision and efficiency. They have developed a fast and noninvasive ultrasound-based technique that shows a patient’s response to chemotherapy very early on. In a study of 100 women with LABC, Czarnota and Sadeghi-Naini found that after just one week of treatment they could predict tumour response with 82% accuracy using their technique. The study was published on Sept. 4, 2017 in the journal Scientific Reports.
“This potentially enables physicians to reach a decision much sooner and say, ‘OK, if the chemo is not going to work, there’s no point in giving someone six months of it. They’ve had it for a week or two; let’s switch it to something else,’” says Czarnota.
The technique is quantitative ultrasound. The researchers, who in the study scanned the women at various points during treatment, have developed a way of using raw data produced and discarded by ultrasound machines to detect whether tumour cells are dying. It works like this: as tumour cells die, the intensity of the ultrasound signal increases about fivefold as it interacts with tissue. Edging past piles of paper in his crowded office, Czarnota begins drawing on his whiteboard to explain. “When a cell dies, the cell’s shape changes. The nucleus condenses and breaks up into little bits,” he says, sketching a blob with small dots inside it. “Sound interacts much more efficiently with this because the density of these nuclear fragments has gone up. So that results in a change in these ultrasound spectra.”
The researchers analyzed features of ultrasound echoes throughout each woman’s tumour and “mapped” where in the tumour cells were dying and to what extent. The “map” provides a big-picture view of patterns of cancer cell death.
The method also predicted outcomes. “We followed these patients for up to five years after treatment and found that patients classified as responders and nonresponders with this technique after one week of treatment demonstrated statistically significant different survival,” says Sadeghi-Naini, speaking to the prognostic utility of the technique.
The method is also being tested at MD Anderson Cancer Center, Princess Margaret Cancer Centre and St. Michael’s Hospital. “We are doing multicentre studies to evaluate the technique at different sites with different users,” says Sadeghi-Naini, adding that they want to ensure that it works regardless of the type of ultrasound system used.
Having worked on this for two decades—first in test tubes, then preclinically and now in patients—Czarnota says they will extend the proof-of-principle research further still by investigating whether use of the technique influences outcomes. What if, very early into treatment, you could spot those people who weren’t responding to a particular drug and try a different tack? That’s just what the researchers will do in their next clinical trial, slated for 2018. “We’re going to launch a study whereby we use this information to tailor the chemotherapy; if [a patient is] not responding, the physician will switch the chemo to something else,” says Czarnota.
In a nutshell
- Scientists at Sunnybrook Research Institute have developed an imaging technique that shows a patient’s response to cancer treatment as early as one week into therapy.
- They analyzed features of ultrasound signals to detect whether tumour cells are dying.
- The technique could enable doctors to determine early on whether a treatment is working and, if not, switch patients to one that might work.