In search of a sign
By Alisa Kim
The Canadian Cancer Society estimates more than 23,000 Canadian men will be diagnosed with prostate cancer this year, representing about 24% of all new cancer cases. Once a diagnosis is made, it is difficult for doctors and patients to make treatment decisions due to the difficulty in predicting how aggressive the disease is and its likelihood of recurrence.
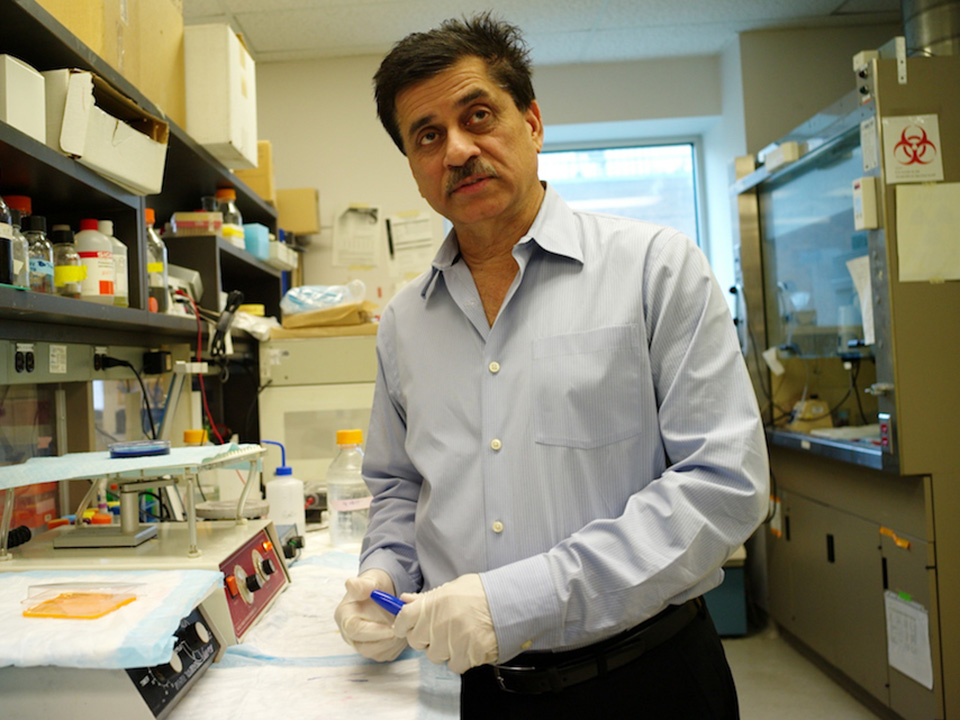
“You can do better clinical management with better biomarkers,” says Dr. Arun Seth, a senior scientist in Biological Sciences at Sunnybrook Research Institute (SRI). “Right now we only have the PSA [prostate specific antigen test]. Everybody’s looking at different types of biomarkers, and molecular biomarkers are better than any other biomarkers. They can give you better information compared to what is out there.”
The PSA test measures the blood level of a protein made by the prostate. The PSA level is often higher in men with prostate cancer; however, some men with the disease do not have elevated levels of PSA. Moreover, noncancerous conditions, including inflammation of the prostate, can cause a man’s PSA level to rise.
Given the limitations of the PSA test, Seth and colleagues, including Dr. Robert Nam, a clinician-scientist at SRI, and Dr. Linda Sugar, a pathologist at Sunnybrook, sought to find prostate cancer biomarkers that could inform a patient’s prognosis. The researchers analyzed the ribonucleic acid (RNA) of tumour samples from 100 patients who underwent radical prostatectomy.
Along with deoxyribonucleic acid (DNA), RNA is found in all cells. It copies genetic information from DNA and translates it into proteins made by the cell. Ribonucleic acid is made up of four different units: adenosine, cytosine, guanosine and uracil (A,C,G and U). The letters and their sequence encode all of our genetic information.
The researchers used genetic sequencing equipment to study the entire expression of RNA in formalin-fixed, paraffin-embedded tissues of patients from three centres in North America: the Atlanta Veterans Administration Medical Center in Atlanta, Georgia; Moffit Cancer Center in Tampa, Florida; and Sunnybrook’s Odette Cancer Centre.
“Peoplehave done [this] on frozen tissues, but the frozen tissues are not good because you don’t have the clinical history of those patients. With paraffin, we had more than 10 years of clinical data for every patient or tumour, so we could then relate our findings with the clinical findings,” says Seth.
Of the roughly 25,000 genes in the human genome, the researchers identified a panel of 24 biomarker genes capable of predicting signs of disease recurrence. Of the 24 genes, 16 have been associated with cancer; five with prostate cancer.
Using clinical information associated with the prostatectomy samples, the researchers validated the 24-gene panel. They also compared it to other biomarker panels and found it outperformed previously published markers. It was also better than using only clinical parameters. “The panel has significant value over other methods in terms of predicting [disease] recurrence. That’s what we discovered,” says Seth. Results of the study were published this year in Cancer Research.
Seth notes that RNA sequencing of biopsy samples is too complex and costly to be done routinely. The researchers are building on their discovery by trying to simplify the test for clinical use.
One way of doing this would be to use droplet digital polymerase chain reaction, a method of measuring the amount of nucleic acid in a sample that has proven useful for studying variations in gene sequences. “You put your [biopsy] sample in the system and it would tell you ‘yes’ or ‘no’ whether those genes are expressed or not,” says Seth.
The researchers will examine the gene panel in detail to see if they can target fewer genes. “We’re also trying to narrow down the panel so that instead of 24, we can drop it down to less than that so it will make it easier for clinicians down the road to use it for diagnostic or prognostic purposes.”