Depression and Heart Disease: New Link Found
Researchers have identified an enzyme that may trigger depressive symptoms in patients with heart disease and may help to explain why general antidepressants are often not as effective for these specific patients.
"Our study confirms that depressive symptoms are associated with inflammation in patients with heart disease and suggests a mechanism by which the brain might be affected," says Walter Swardfager, lead author of a new study and PhD candidate in the neuropsychopharmacology research program at Sunnybrook.
The research focuses on an enzyme that is part of the inflammatory process in patients with coronary artery disease (CAD). The enzyme breaks down the amino acid tryptophan and it is associated with damage to brain cells. Findings show a significant association between activation of this enzyme and the degree of depressive symptoms in these patients. They also identify a trend towards even higher levels in those suffering from clinical depression.
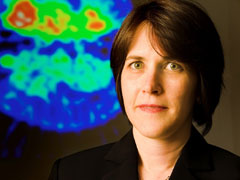
"This enzyme makes ‘brain unfriendly' chemicals," says Dr. Krista Lanctôt, principal investigator and head of the neuropsychopharmacology research program at Sunnybrook. "We are trying to chase down a treatment for patients with CAD that will block the enzyme and/or prevent the inflammatory process in the first place."
This study adds to a growing body of evidence that suggests depression worsens heart disease; in fact, it is shown to be even more of a risk factor for mortality than traditional cardiac risk factors such as high blood pressure. The prevalence of depression in patients with CAD is shown to be much higher than that of the general population, contributing to a poorer quality of life and increased mortality.
"The challenge is that a large number of patients with CAD do not respond well to traditional antidepressants, and for those who've tried everything, we need new options specifically tailored to them," says Dr. Lanctôt. "The first step was to prove that this pathway is involved, and now we need to try to stop it. We hope to find a drug that can meet this specific need."
PDF / View full media release »