Together we can accelerate the understanding, treatment and care of brain disorders
By 2020, brain disorders are expected to be the leading cause of death and disability in Canada. We aim to change this.
Sunnybrook’s Hurvitz Brain Sciences Program is taking the lead in solving the biggest threats to brain health: stroke, dementia and mental illness.
We are unique amongst Canadian brain sciences programs. Some programs address mental illness alone, some conduct only research, some provide only clinical care and some focus on one specific age group. We are the only program that brings all of this together into one fully integrated effort.
We are building the Hurvitz Brain Sciences Centre to be a hub for patient care research and teaching. It will be a centre where collaboration among our brain sciences experts will spark new discoveries and bring new innovative treatments to patients sooner.
Here’s how:
Unprecedented collaboration across disciplines – brain disorders will not be understood by just one medical specialty
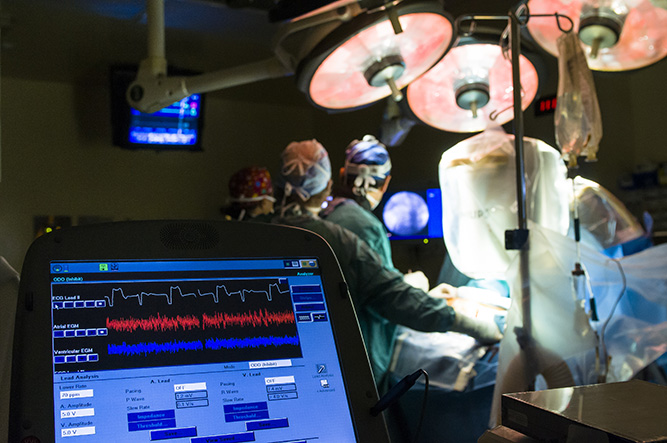
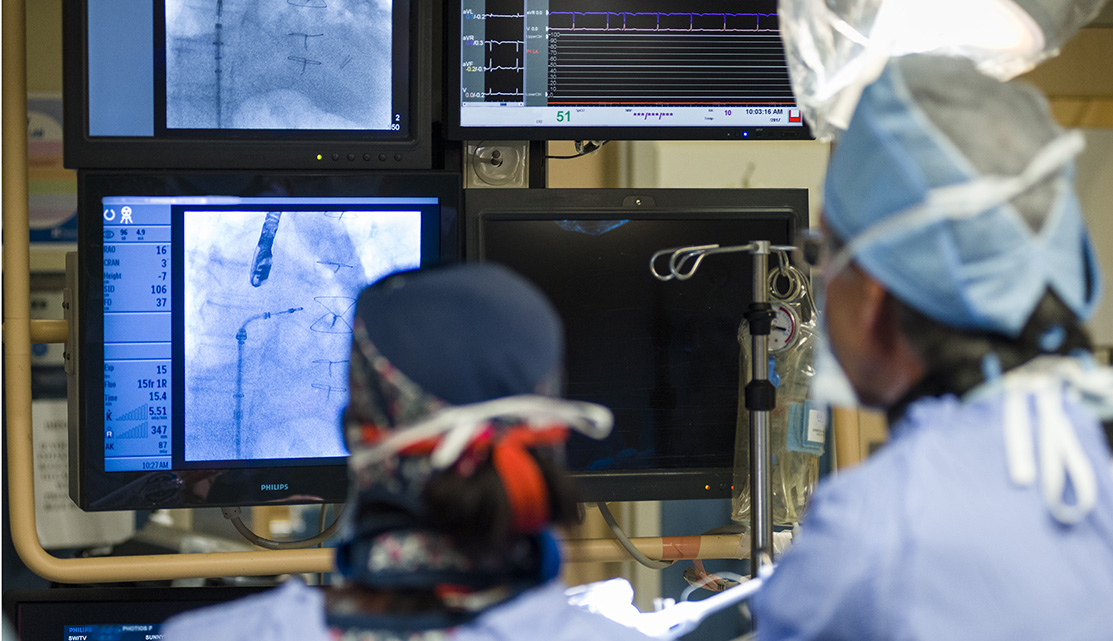
Our neurologists work alongside psychiatrists. Our neurosurgeons work alongside brain imaging specialists. Our psychiatrists work alongside pharmacologists.
Why? Because each specialty teaches us lessons about the others, thereby accelerating research that will return patients to their families faster and healthier than before.
Care throughout the lifespan – from adolescence to the senior years
Our experts from the Hurvitz Brain Sciences Program care for people at all stages of life. Most discoveries made in one age group translate to the others, ultimately impacting all ages.
Integrating psychiatry and the other brain sciences
By integrating psychiatry and the other brain sciences, we take psychiatry out of the shadows and shine a light of understanding on it. Mental illness should be treated like any other medical condition.
Embedding research in patient care
Uniting research with patient care means patients receive new treatments sooner. Our ultimate goal is to improve outcomes and restore patients to health as quickly as possible.
Our aim is to provide the clinical care, research, leadership and education needed to confront one of the largest health threats of our time: disorders of the brain. We have the teams in place. We have the expertise. And we have the technology.
Now, we need the community’s help in creating a new centre that will accelerate the understanding, treatment and care of people with brain disorders.
Watch: Learn more about the centre from patients and Sunnybrook brain specialists
Download more information






 \
\