How to make multiple pregnancies safer

Research team is making inroads on reducing the risks for women carrying twins (or even more babies)
September 12, 2018

Twins Rey and Ron Walters, born at 26 weeks’ gestation, are among the preemies delivered at Sunnybrook, one of the largest multiple-babies birthing centres on the continent.
Photographed kneeling among an elaborate presentation of blossoming flowers, Beyoncé stuns. Surrounded by captivating colours, she is dressed in lingerie and draped in a pastel green veil; however, the focus of the highly stylized image, which the multi-Grammy winner shared on Instagram in February 2017, isn’t the amount of skin she’s showing—it’s the baby bump she’s cradling in her hands. Via the accompanying caption, she reveals she is expecting twins. In June 2017, Rumi and Sir Carter joined a growing number of twins in North America.
On Canadian soil, more than 6,000 sets of twins are born each year, contributing to the current rate of multiple births, which is roughly one in 31. A multiple birth is defined as a birth in which two or more babies are delivered from a single pregnancy on the same occasion. As per 2013 numbers from Statistics Canada, 3.3% of live births in the country were multiples, a 1.2% increase from 1993.
Twin pregnancies are associated with serious adverse outcomes, one of which is preterm birth. The World Health Organization defines preterm birth as one in which a live baby is born before 37 weeks of pregnancy is completed. A normal gestation period is 37 to 41 weeks. Roughly 15 million babies are born prematurely every year worldwide, and the number is growing. Complications arising from it, including respiratory distress syndrome, chronic lung disease and cardiovascular disease, are among the leading causes of death for children aged under five years. It’s estimated nearly one million deaths globally were a result of preterm birth in 2015. In this country, there were 29,716 preterm births in 2013, or 7.8% of total births.
The rise of preterm birth can be attributed to a few issues, Dr. Nir Melamed says. “There are many changes that happen at the level of population. Women are more likely to postpone childbearing, and we know that a more advanced maternal age can predispose to complications leading to preterm babies. There’s also an increase in the prevalence of obesity, which can predispose to complications that result in prematurity,” the associate scientist in the Women & Babies Research Program at Sunnybrook Research Institute (SRI) says.
The last issue he underscores circles back to multiples. “More people are now using fertility treatments, which often result in twin pregnancies. Twin pregnancies are a major risk factor of prematurity. Even though only 1% to 3% of pregnancies are twins, twins are responsible for 25% to 35% of all cases of prematurity. Some people are happy about having two babies at the same time—it’s an efficient way to increase your family—but it’s pretty risky.”
There are three categories of premature babies, grouped by how early they’re born. Infants born between 32 and 37 weeks’ gestation are moderate to late preterm; those born between 28 and 32 weeks are very preterm; and those born before 28 weeks of pregnancy—the smallest and sickest babies—are extremely preterm. Sunnybrook cares for infants in all three sets.
To understand the biology of multiples and predict women at risk of preterm birth, scientists in the Women & Babies Research Program at SRI are pursuing several research ventures under the guidance of Dr. Jon Barrett. A senior scientist and director of the program, Barrett spearheaded the landmark twin birth study, which proved that vaginal birth is as safe as caesarean section for women pregnant with twins. Before this, and based on weak evidence, Barrett notes, the prevailing belief was that C-sections were safer. The pioneering study profoundly informed obstetrical care worldwide when it was published in The New England Journal of Medicine in 2013. The decade-long massive undertaking involved 2,804 women with twin pregnancies across 106 centres in 25 countries. “There will never be another trial like this,” Barrett, who is also a professor at the University of Toronto, says.
As central as Barrett is to multiples and preterm birth research at SRI, he is nonetheless preparing the next generation of scientists to take the reins. “I’m not going to be around forever—I have to think about the future. I needed to find someone like I was 20 years ago; I found someone better,” he says. The person he’s referring to is Melamed, whom he recruited. “He’s got the same energy and enthusiasm, but he’s much smarter than I ever was. Nir has the same love for twins as I do, so he’s taking over [this area of research].”
Melamed explains the significance of Sunnybrook for multiples research: “Dr. Jon Barrett established the Twins Clinic here many years ago, which puts us in a unique position to answer questions. We have large populations of twins coming to Sunnybrook—it’s one of the largest twin centres in North America. What we want to do is study various aspects of twin pregnancies.” The maternal-fetal medicine specialist at Sunnybrook and associate professor at U of T elaborates: “We study preterm birth in twins, investigate the growth of twins compared with singletons, conduct studies on diabetes and pre-eclampsia in twins, and so forth.”
Because multiples and preterm birth are so tightly intertwined, the research of Melamed, Barrett and colleagues can be categorized broadly as projects aiming to identify early which women might be at risk of premature delivery, and those seeking to reduce negative outcomes associated with it.
Melamed says identifying women at risk of premature birth is easy when they have contractions or are in pain; contrarily, detecting such women when they don’t present with symptoms is tricky. Enter repeated cervical length measurements. Cervical length is measured in women pregnant with twins via transvaginal ultrasound once at 20 weeks’ gestation. Then, a decision is made if she’s at risk of early delivery based on whether the cervix has shortened. Melamed and Barrett, however, believe a single measurement isn’t enough. “It’s not sufficient to assess the cervix only once. In some cases, the measurement might change later on in pregnancy; not necessarily at 20 weeks, but instead at 24 or 26 weeks,” Melamed says.

Dr. Jon Barrett, with twins Onyx and Nasir Anderson-John, and their parents Deborah Anderson and Khadel John. The twins, who were kept in the neonatal intensive care unit for two months, weighed 2 pounds each when they were born at 29 weeks and six days of gestation.
To see whether early birth could be forecasted by measuring the length of the cervix more than once, they took serial measurements of asymptomatic women pregnant with twins at mid-gestation and every two to three weeks thereafter until 28 to 32 weeks’ gestation. The main discovery by the investigators, which included Dr. Roberto Romero, chief of the perinatology research branch at the National Institute of Child Health and Human Development in the U.S., was that serial measurements predict preterm birth in women pregnant with twins better than does a single measurement. “With the use of serial measurements we can identify many more women who are at risk of preterm birth who may benefit from preventive interventions; many of these women would have been missed if we were to use only one measurement,” Melamed says. Published in the American Journal of Obstetrics & Gynecology, the findings were well-accepted and highly cited, he adds. The goal now is to find other tools or biomarkers that can be used alongside serial measurements of the cervix to improve prediction.
Identifying women at risk of preterm birth as early as possible is also a goal of Dr. Phyllis Glanc’s, an associate scientist in the Women & Babies Research Program at SRI and a radiologist at Sunnybrook, one of five radiologists partnering with maternal-fetal medicine specialists at the hospital. Working in conjunction with Barrett and Melamed, Glanc, who is also an associate professor at U of T, is studying whether utero-cervical angle (UCA) measurements, captured via ultrasound, can be used to predict early labour.
Typically, before a mother delivers, her cervix is at a 90-degree angle at the base of her uterus, forming a reverse “L” shape. “As [a woman goes] into labour, the cervix not only shortens and opens, but the angle goes from 90 to 180 [degrees] to give the baby an exit route,” says Glanc, who is the specialty chair of the women’s imaging section on the American College of Radiology Appropriateness Committee, a rare position for a Canadian to hold. Her team is looking into whether UCA measurements close to 180 degrees at 24 to 29 weeks’ gestation indicate a woman is at risk of early delivery.
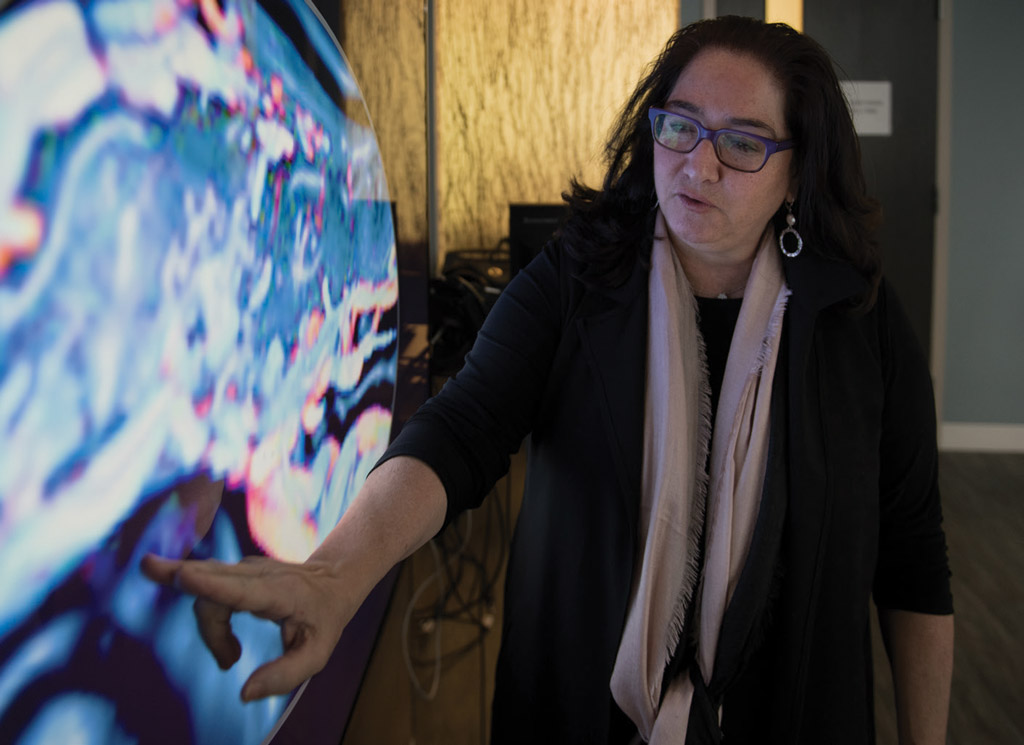
The placenta is among Dr. Phyllis Glanc’s research areas in her pursuit to predict and prevent early birth.
Thus far, results suggest a trend in the 76 women studied, whereby larger UCA measurements do point to higher rates of premature birth. She notes that more cases need to be assessed, however, before she can come to a firm conclusion.
The placenta is also a focal point for SRI researchers. One of the most vital organs in pregnancy, the placenta is rich in biological information and serves as the lifeline between mother and baby—or babies. “Think of it as a black box,” Melamed says. “After the baby is delivered, the placenta is delivered as well. By examining the placenta, we can understand what processes happened—whether there was an infection, insufficient blood flow to the placenta or bleeding from the placenta.”
A debate that rages among those in the maternal-fetal medicine community is whether smallness in twins is caused by placenta-mediated factors, as it is in singletons who are born small. In this case, small describes a baby whose birth weight is less than the 10th percentile. To address this, Melamed and Barrett enlisted Dr. Christopher Sherman, a pathologist at Sunnybrook, to help investigate the placentas of small twins and small singletons. “Based on our study, as well as other studies, we believe that the slower growth of twins compared with singletons that is observed starting at about 28 weeks is in many cases not due to failure of the placenta, but instead due to adaptation of the twins to the more crowded intrauterine environment,” Melamed says. He adds, “This adaptation may buy the twin fetus more time in utero at the expense of slower growth.”
The trio also worked together to determine whether there is an association between placental blood flow abnormalities and low birth weights of the nonpresenting fetus—the twin farthest from the cervix—in dichorionic [di-kor-ee-on-ik] twin pregnancies, or twins with separate placentas. Looking at over 1,300 women who delivered these types of twins between 2002 and 2015, they noted a correlation between low-birth-weight nonpresenting babies and less blood flow to those babies. The work was outlined in Obstetrics & Gynecology. Barrett says the goal is to use advanced technology such as ultrasound texture analysis to determine when nonpresenting babies may be at risk of low birth weight before they’re born and then intervene. “If we can tell that these babies have [placental] abnormalities, maybe we can do something about it; maybe we can give a drug to increase blood flow. That’s why this is really important.”
Glanc sees potential in studying the placenta, too. In her work with Barrett on women pregnant with twins in separate placentas, they, along with colleagues, added a test to their routine exams between 11 and 14 weeks’ gestation to gather 2-D and 3-D measurements of the organ. They were interested in learning whether the insertion point of the umbilical cord in the placenta might contribute to fetal growth restriction, which in turn could cause premature birth. Babies deemed to be at risk of fetal growth restriction might be delivered early because they have a higher chance of stillbirth. “When life is good, the umbilical cord inserts right in the centre [of the placenta], so nutrition spreads out evenly. In singletons, there is some evidence to suggest that when the umbilical cord inserts at the edge, it’s bad,” Glanc says.

Dr. Nir Melamed, who says twin pregnancies are responsible for at least 25% of all cases of prematurity, a rate his research seeks to slash, helped care for Rey and Ron’s mom, Camiele Walters.
If umbilical cords insert in placentas at the edges, meaning there is a short distance between the insertion points, then Glanc asked whether that could lead to weak nutrition flow throughout the placenta and consequently adverse outcomes. Her second question, which looked to 3-D measurements for answers, was whether a smaller placenta similarly led to an adverse outcome. The team, which includes Barrett, is awaiting the birth of some babies in the study and will need to recruit more participants before they can draw a definitive conclusion, but Glanc says a trend in the data has emerged that confirms her suspicion. It seems when the distance between two cord insertion sites is shorter—when the cords don’t insert in the middle of two placentas, but instead on the periphery—there’s an increase in fetal growth restriction, which could result in stillbirth, preterm delivery and other health issues.
Glanc has joined forces with Melamed and Barrett to look at aspects of the cervix other than length. They have teamed up with Dr. Anne Martel, a senior scientist and physicist in the Odette Cancer Research Program at SRI, who is an expert in image analysis and machine learning. “We know that the shorter the cervix is, the higher the risk is of preterm birth, but looking just at the length is quite limited,” Melamed says.
Changes occur to the cervix at a structural level during pregnancy and include softening and tissue breakdown, Melamed says. “The software looks at many tiny features of the image—things we cannot see with the bare eye—and identifies patterns within the ultrasound image of the cervix. Then, we use machine-learning algorithms to analyze these patterns and identify women who might be at risk,” he says.
The proof-of-concept unpublished study, done last year, used images of 98 women’s cervixes taken at 22 and 26 weeks of gestation. With these data in hand, Melamed says the next step is to validate the results prospectively by running the algorithm on more images and determining if it’s an accurate tool to predict adverse outcomes. “This is important because ultrasound images are great; they’re cheap, and everyone does them. It would be helpful if you could predict that someone was going into preterm delivery, so you could appropriately manage that patient and make sure they’re taken care of,” says Martel, who is also a professor at U of T.
Another promising area of research involves medication. To prevent complications associated with preterm birth, Melamed and Barrett turned to antenatal corticosteroids. Given to pregnant women to decrease neonatal morbidity and death by making the baby’s lungs more “mature,” as Melamed says, antenatal corticosteroids are highly effective in neonates of a size appropriate for their gestational age; however, their usefulness is unclear in preterm babies that are small for their age, or of a birth weight that’s less than the 10th percentile. To test if the drug has similar benefits in fetuses of all sizes, they collected data on more than 6,500 newborns in Canada between 2010 and 2014.
They found that when antenatal corticosteroids were given to pregnant women who delivered preterm babies that were small for their gestational age, rates of neonatal death were lower than among babies whose mothers didn’t receive the intervention. Further, the study showed that benefits of the drug are maximized when given to the mother no earlier than seven days before delivery. “If the baby is born more than seven days after administration, [the drug’s] beneficial effect decreases by 50%,” Melamed says. Should corticosteroids be delivered, timing needs to be optimized, he adds. The results were published in Obstetrics & Gynecology.
Navigating the waters encompassing multiple and preterm births can be disheartening at times, Melamed says. “In many cases we feel a bit frustrated in our ability to help women who we know are at high risk of preterm birth. We have a very limited set of interventions. That’s why this [work] is very important.” Emphasizing his interest in multiples, he adds, “Twins are very high-risk pregnancies, and they’re prone to many complications—not only preterm birth, but also high blood pressure and diabetes. Most of the studies done so far on the mechanisms of pregnancy complications focused on singletons, so that we don’t have a good understanding of how we should approach these conditions in twins.”
Multiples by the numbers

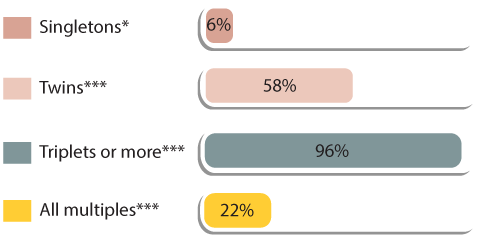
*Statistics Canada (2013)
**Multiple Births Canada, Preterm, Low Birth Weight and Multiple Births: An Information Guide for Parents (2005)
***Multiple Births Canada, Multiple Births Facts & Figures (2011)
Barrett holds the Fred Waks Chair in Maternal-Fetal Medicine Research at Sunnybrook.



