Writing the skin
Team develops hand-held device that can deposit wound-healing tissue directly onto severe burns
“Nature is very clever. It usually outsmarts humans quite significantly,” says Dr. Marc Jeschke, a senior scientist in Biological Sciences at Sunnybrook Research Institute (SRI). He is speaking about the challenges of engineering skin, the body’s largest organ and bulwark against environmental assault.
Also a burn surgeon and director of the Ross Tilley Burn Centre at Sunnybrook, Jeschke isn’t backing down from this challenge. He is working with researchers at the University of Toronto, where he is a professor in the departments of surgery and immunology, to develop a hand-held skin printer. Weighing less than two pounds and resembling a packing-tape dispenser, the skin printer was designed in the lab of Dr. Axel Guenther, an associate professor in the department of mechanical and industrial engineering at U of T, by his PhD student Navid Hakimi. The “bio-ink” is a mixture of cultured cells and proteins. In April 2018, the team published a proof-of-principle study in the journal Lab on a Chip showing that the device can produce skin tissue sheets to cover wounds in preclinical models. Jeschke’s role was overseeing the biological studies, all of which were done at SRI.
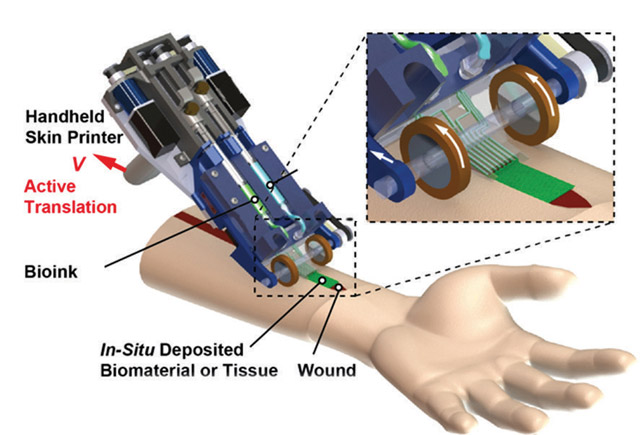
A rendering of the skin printer that is being developed in the lab of Dr. Axel Guenther in collaboration with Sunnybrook Research Institute senior scientist Dr. Marc Jeschke.
The collaboration between Jeschke and Guenther began about five years ago. The skin-printing technologies they have worked on have come a long way. The first printer “looked like a fish tank,” says Jeschke, noting the process has been iterative. The early versions were not designed for use at the point of care. “The problem with that is [the skin] is very fragile. How do you carry something that’s printed and looks like a patient’s skin to the operating theatre and put it on a patient? There are many steps in between. Now we [could] print it directly on a patient,” he says.
The clinical need is dire. A third-degree burn, caused by scalding liquid or flames from a fire, for example, destroys skin’s outer layer and hair follicles. Once gone, new skin will not grow. The only treatment for deep burns is to take healthy skin from elsewhere on the body and transplant it to the site of injury. This procedure, called split-thickness skin grafting, results in longer hospital stays, creates more wounds and poses a risk of infection. “Skin is very thin, and it’s being used over and over. It’s not ideal, but it’s currently the best we have,” says Jeschke. Sunnybrook cares for most people in Ontario who have burn injuries—about 300 people annually. Jeschke estimates the burn centre team conducts thousands of split-thickness skin grafts each year.
Other researchers have grown skin substitutes, but the resulting products are not functional, says Jeschke. They blister, and lack pigment and sweat glands. The biggest problem by far, though, is that they take too long to make. A wound from a large burn needs to be covered quickly. “Waiting six to eight weeks is not feasible,” Jeschke says. In addition to depositing skin directly on top of a wound, the handheld skin printer works fast. As long as there are sufficient quantities of cells, the printer can produce tissue sheets within minutes.
The next step is to determine the best source and exact composition of the bio-ink. The goal is to use complex and varied cell types like melanocytes, keratinocytes and fibroblasts, as well as sweat glands, to mimic human skin. Whatever the source, for example, from a patient’s biopsy sample, they will need a lot of cells, notes Jeschke. They will then test the formulation clinically to see whether the technology improves wound healing. Jeschke surmises that clinical trials are several years away. “This is just the delivery vehicle,” he says. “Now it’s up to us to study whether, biologically, we can add the components to make this into good, functional skin.”
— Alisa Kim
This research was supported by the Canadian Institutes of Health Research, U.S. National Institutes of Health, Natural Sciences and Engineering Research Council of Canada, and Toronto Hydro. The Canada Foundation for Innovation provided infrastructure support through the Centre for Research in Image-Guided Therapeutics.



