MRI technique holds key to selecting patients for heart treatment
New method of identifying hard versus soft lesions shows promise for people with peripheral arterial disease
Peripheral arterial disease (PAD) occurs when arteries carrying blood to the limbs become blocked. For the roughly 800,000 Canadians affected by PAD, endovascular treatment offers a less invasive method to restore blood flow than does traditional bypass surgery. During an endovascular procedure, a guidewire is used to locate the blockage, so that a balloon or a metal scaffold called a stent can be inserted to prop open the vessel.
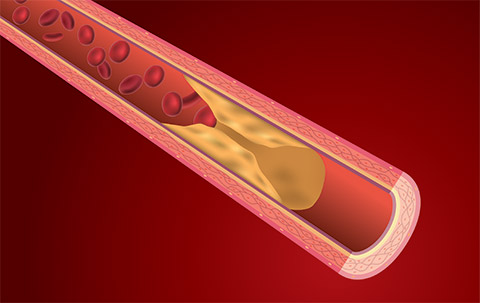
Image: Getty Images
Not all lesions can be treated this way, however, because some are simply too hard to penetrate. Indeed, 20% of these endovascular procedures fail immediately due to the inability of the guidewire to pass through. Predicting which blockages cannot be opened with a balloon or stent has, until now, been impossible, leading to delays in effective treatment and potentially worse outcomes.
To solve this problem, Sunnybrook vascular surgeon Dr. Trisha Roy developed an MRI technique that can identify which lesions are more difficult to cross. Working in the Schulich Heart Program with vascular surgeon Dr. Andrew Dueck, along with Dr. Graham Wright, director of research for the program at Sunnybrook Research Institute, Roy tested the method on 14 patients with PAD, all of whom had MRI before having the endovascular procedure.
In patients whose lesions were identified as hard by MRI, it took nearly 15 minutes for the guidewire to pass through, and more of these patients required a stent. In contrast, the crossing took just over two minutes in patients who had soft lesions, as shown on the MRI. Findings were published in the Journal of Vascular Surgery.
The study highlights the potential utility of MRI for selecting the most appropriate patients for endovascular treatment.



