Good Manufacturing Practices facility is bridge to clinical translation
Before a therapy reaches people in need, it must go through rigorous tests, including clinical trials. For it to get to this stage, however, it must be manufactured in a government-approved environment to ensure an exceptionally high standard of production quality is met. At Sunnybrook Research Institute (SRI), that environment is the Good Manufacturing Practices (GMP) facility.
“Good manufacturing practices are regulations that the government has put in place for anyone manufacturing drugs, food products, contraceptive devices, medical devices and so forth. They need to make sure these products are safe and that quality is embedded in the product throughout its life cycle, rather than someone trying to push quality into the product after it’s been manufactured,” says Nickett Donaldson-Kabwe, operations manager of the GMP facility at SRI. She notes that gene and cell therapy products make up most of the work she sees. These fall under the domain of regenerative medicine, which is the regrowth, repair or replacement of defective cells, organs or tissues.
The GMP facility offers four classified controlled cleanrooms, which have air that is at least 1,000 times cleaner than outside air. These rooms allow users to isolate, expand and bank cells. “What that means is someone can come in and say, ‘I only have one vial of this stem cell, but I want 300.’ We train them on proper cleanroom procedures, so gowning etiquette, sanitation, equipment use, et cetera, and this enables them to process and manufacture their cells under aseptic conditions,” Donaldson-Kabwe explains. Scientists in this field are working toward instructing stem cells to become specific cells that can be injected into people to treat disease.
Each cleanroom is made from specialized antimicrobial materials that don’t rust. Further, the panels in the rooms can be removed and replaced if damaged. The rooms are closely monitored to ensure that products created in the space are safe and pure. The volume of air in each room is exchanged more than 260 times per hour to ensure it is always clean, and the air filters are tested every six months as per GMP guidelines. The rooms are cleaned monthly if not used or directly after use. They are recertified yearly.
Prior to using the GMP facility, a person must complete training, which the facility provides. Protocols, most of which are developed by Donaldson-Kabwe, include strict guidelines around hygiene, like gowning up and disrobing, and rules around equipment brought through the doors; everything must be sanitized and certified. “If it’s considered critical to someone’s manufacturing, it has to undergo a qualification process,” she says.
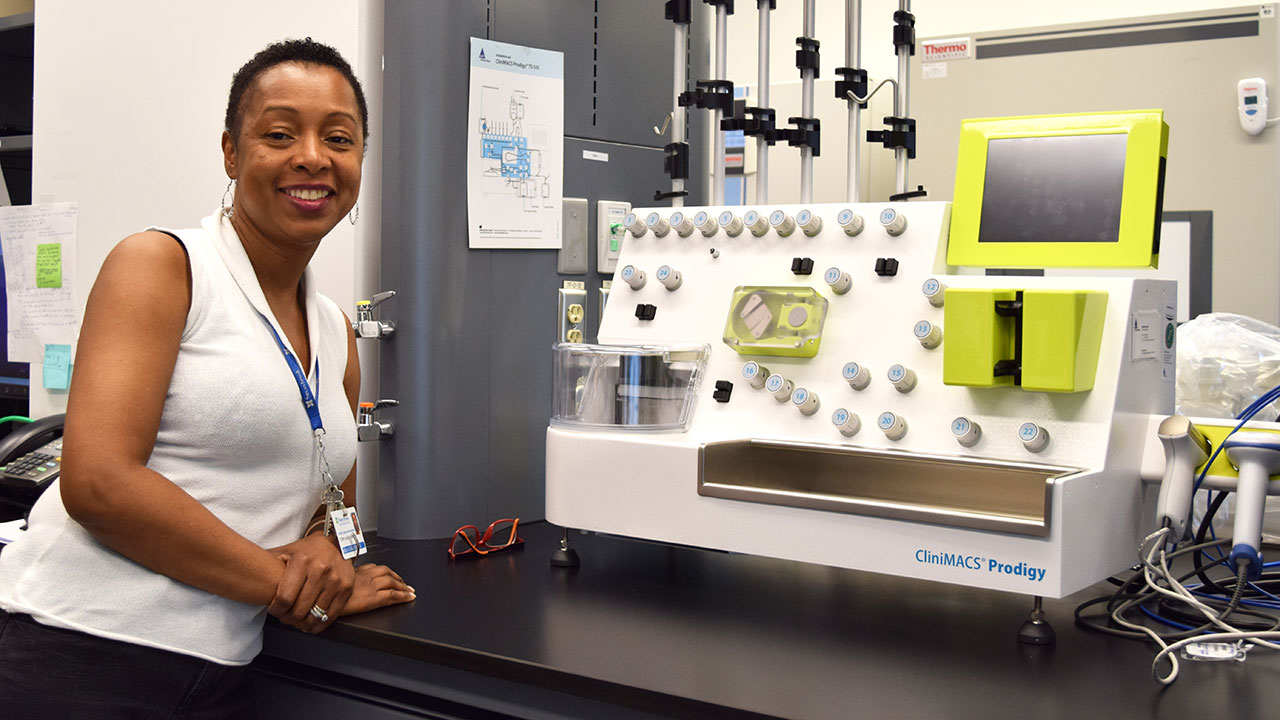
Outside the cleanrooms, there sits an instrument called the CliniMACS Prodigy that allows users to manipulate cells for a targeted purpose. Donaldson-Kabwe says one of its uses is to develop gene therapies. It works like this: Researchers extract cells from a person with a given disease. Next, the machine is used to sort the cells and isolate the defective ones causing the condition. Then, a gene that researchers think might fight the condition and restore function in the person is injected into the defective cells. Finally, large quantities of these new cells are made and delivered to the person.
Users come from near and far
Dr. Charles Cunningham, a senior scientist in Physical Sciences at SRI, is using the facility. In one of his projects, he is making an MRI contrast agent to detect early-stage heart failure. An MRI contrast agent is a chemical substance that when injected into a person makes it easier to image inside the body or brain. He is also exploring whether this agent can show if therapies are effective in cases where cancer has spread beyond its site of origin.
Dr. Juan Carlos Zúñiga-Pflücker, a senior scientist in Biological Sciences at SRI, aims to be a user in the future. “We have a plan to one day use the GMP facility to make pro-T cells using our new technology for inducing T cell development from stem cells,” he says. T cells are white blood cells that are essential to the immune system, while pro-T cells, otherwise known as progenitor-T cells, are early T cells—they originate in the bone marrow before traveling to the thymus to become fully functional T cells. “I am very excited to be able to move our finding to the clinic, all within SRI,” Zúñiga-Pflücker adds.
The GMP facility is also available to external groups. People from academia and industry are users, some with headquarters in the U.S. “The facility is expensive to operate. To offset some of the costs, and to make it more affordable for the academic community, we accept some private sector projects,” Donaldson-Kabwe says. As of summer 2019, the facility was at capacity. She adds that the interest external communities have expressed took her by surprise. “We didn’t realize how much of a need there was.”
Scheduling projects has its challenges. Some users prefer to book one of the cleanrooms for more than a year, while others might request use for a couple of weeks. Donaldson-Kabwe says, “We sort of gauge when projects will be coming in so we know how long we can book a room for. We try to accommodate as many [projects] as we can, but we also have to be strategic—we don’t want a room sitting empty in anticipation of a project that never comes.”
Open for business: taking therapies to the clinic
The GMP facility at SRI, built as part of the Centre for Research in Image-Guided Therapeutics, and funded primarily by the Canada Foundation for Innovation, has been operational for five years. Donaldson-Kabwe developed it from infancy to its fully functional, highly sought-after current state. Kevin Hamilton, director of strategic research programs at SRI, says the suite was born out of a need to enable researchers to develop new therapies on-site. He notes those involved in launching the facility include the late Dr. Dan Dumont, who was a senior scientist in Biological Sciences; Dr. Graham Wright, a senior scientist in Physical Sciences; and Zúñiga-Pflücker.
“What [the facility] allows you to do is run clinical trials at a level Health Canada can accept as being real world,” Hamilton says. “Health Canada can be comfortable that the test environment is as good as the commercial pharmaceutical environment.” Hamilton also mentions Dr. Marc Jeschke, a senior scientist in Biological Sciences at SRI, as a soon-to-be user. Jeschke is developing a stem cell therapy to treat burns.
If there’s one thing Donaldson-Kabwe wants people to know, SRI-affiliated or otherwise, it’s that the GMP facility is open for business. “I want scientists to know they can come to us. Space may not be available right away, but they can put their name in, and we’ll review their project to see what we can accommodate and when.”
Asked why it’s important to have a GMP facility at SRI, Donaldson-Kabwe is quick to respond. She notes that GMP facilities are not all that common. In Ontario, apart from SRI’s, there’s a new one in downtown Toronto, at the University Health Network, and one at the Ottawa Hospital Research Institute. Further, she explains, when an investigator submits an application to carry out a clinical trial, they need to outline the resources they have at their disposal. “It puts them in a unique position if they can say, ‘I have my lab here, and I also have access to a manufacturing suite … and I also have access to a clinic.’ It’s strategic to have everything under one roof,” she says.
She adds, “There’s a definite need for facilities of this nature, because you can’t take a product directly from the lab to the clinic. There’s a gap there, and we’re the bridge.”
In a nutshell
- The Good Manufacturing Practices facility at Sunnybrook Research Institute lets users generate therapies for human use in a clean environment that satisfies Health Canada standards.
- New cell and gene therapy products are manufactured to the highest standards.
- The facility, one of only three in an Ontario research hospital, plays a crucial role in taking therapies from the lab to the clinic.